Research Article
Prospective Clinical Study to Find out Epidemiology of Xerophthalmia in Children in a Tertiary Care Centre in India

Deepak Mishra1*, Megha Gulati2, Prashant Bhushan1, Nilesh Mohan2 and Bibhuti Sinha P2
1Department of Ophthalmology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, UP, India2Regional Institute of Ophthalmology, IGIMS, Patna, Bihar, India
*Address for Correspondence: Dr. Deepak Mishra, Assistant Professor in Ophthalmology, Department of Ophthalmology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, UP, India, Tel: 91-9415360338; Email: [email protected]
Dates: Submitted: 24 November 2017; Approved: 28 December 2017; Published: 29 December 2017
How to cite this article: Mishra D, Gulati M, Bhushan P, Mohan N, Sinha PB. Prospective Clinical Study to Find out Epidemiology of Xerophthalmia in Children in a Tertiary Care Centre in India. Int J Clin Exp Ophthalmol. 2017; 1: 066-070. DOI: 10.29328/journal.ijceo.1001010
Copyright Licence: © 2017 Mishra D. et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Vitamin A deficiency; Xerophthalmia; Epidemiology
Abstract
Objective: To study the epidemiology of xerophthalmia in children 2-6 years of age in North India.
Methods: A prospective clinical study was done at two tertiary care centers of North India between 2010 to 2016, Cases were selected from routine OPD and children less than 6 years of age were examined by an ophthalmologist. Diagnosis and classification of Xerophthalmia was done according to WHO classification. All the data recording demographic profile, socioeconomic status, other health problems etc were recorded in a fixed proforma. Data was analyzed by SPSS version 16.
Findings: Two thousand nine hundred forty six cases were included in the study after satisfying inclusion and exclusion criteria. The prevalence of night blindness was estimated to be 2.93% (95% Confidence Interval [CI]: 2.53-3.33) among children between 2 and 6 years of age. Xerophthalmia prevalence was 4.43% (95% CI: 4.19-4.67). Prevalence was more in girls than boys and higher in low socioeconomic status.
Conclusion: Vitamin A deficiency is recognized to be a severe public health problem leading to corneal opacity and childhood blindness in most of the areas of North India
Introduction
Xerophthalmia/ dry eye refers to all ocular manifestations ranging from night blindness to corneal melting due to vitamin A deficiency. Recognition of symptoms and signs of Xerophthalmia and prompt treatment according to the International classification is the mainstay of the therapy. Children & pregnant women are primarily at risk. Xerophthalmia is the most common, most devastating ocular disease attributing to nutritional deficiency. Although xerophthalmia literally means “dry eye,” it denotes the entire spectrum of ocular abnormalities arising from vitamin A deficiency. These include night blindness, retinopathy, conjunctival and corneal xerosis, corneal ulceration and melting, and less obvious alterations in the epithelial structure of the eye and several other organs.
The importance of vitamin A for normal host resistance and survival has become increasingly evident. Even children with mild, subclinical deficiency are at increased risk of respiratory disease and diarrhea, anemia, growth retardation, and death [1]. Although the ocular complications of deficiency are best known and clinically evident, they represent only one facet of this multisystemic disorder.
Some 250 million preschool children are at risk of vitamin A deficiency, mainly in developing countries because of insufficiently varied diets, poor maternal education and inadequate hygiene [2]. Vitamin A Prophylaxis Programme was launched in 1970 with the objective of reducing the disease and preventing blindness due to Vitamin A deficiency. It was initially started in 7 states with severe problems. Later it was extended to the entire country. Under the programme, children aged 6 months to 6 years were to be administered a mega dose of vitamin A at 6 monthly intervals. To prioritize Vitamin A administration, the programme was revised to give 5 mega doses at 6 months intervals to children 9 months to 3 years of age. In view of adequate supplies of Vitamin A, the target group has been revised to cover children 9 months- 5 years, since 2007.Shervin et al reported that the prevalence of Xerophthalmia has been declining, because of widespread vitamin A supplementation and measles immunisation in at-risk populations [3]. Bahreynian et al also reported reduction in disability-adjusted life years due to vitamin a deficiency in Iranian population aged less than 5 years [4]. The objective of the present study was to determine the epidemiology of vitamin A deficiency in children aged 2-6 years in north India.
Materials and Methods
A prospective clinical study was done at two tertiary care centers of North India between 2010 to 2016, Cases were selected from routine OPD and children less than 6 years of age were examined by an ophthalmologist. Diagnosis and classification of Xerophthalmia was done according to WHO classification. All the data recording demographic profile, socioeconomic status, other health problems etc were recorded in a fixed proforma. Seeing the prevalence of disease, we use a 99% confidence level, a 50% standard of deviation, and a 5% margin of error to calculate the sample size. Data was analyzed by SPSS version 16.
A pretested questionnaire was administered to mothers or female caregivers, in order to collect demographic and health information on the children studied and on socioeconomic and environmental factors of relevance to the households. The child’s dietary vitamin A intake was assessed with the help of a semi quantitative food frequency questionnaire. Anthropometric measurements, ocular examinations and vitamin a status estimation was done.
Height and weight were measured without footwear. Children were classified as underweight, stunted and wasted if the calculated weight-for-age, height-for-age and weight-for-height Z-scores respectively were below -2.0 standard deviations. Ocular examinations were conducted by an ophthalmologist. The various stages of xerophthlamia were identified and information on night blindness was collected. Diagnosis, classification & treatment of Xerophthalmia was done according to WHO classification & guidelines.
Results
Two thousand nine hundred and forty-six childrens were included in the study with higher prevalence in girls than boys. Female children’s were predominated in the study, fifty-nine percent were female whereas forty-one percent were male. Higher number of participants were from in low socioeconomic status (According to Kuppuswamy scale) the prevalence of night blindness was estimated to be 2.93% (95% Confidence Interval [CI]: 2.53-3.33) .Overall Xerophthalmia prevalence was 4.43% (95% CI: 4.19-4.67).In 46% cases more than one child was affected in the family. Our study also found that 63.7% children received no treatment because of lack of knowledge & awareness. However 27.8 % were taking treatment from local doctor or health worker which did not contain Vitamin A Supplement. Stool microscopic examination of children showed 23% children were suffering from worm infestations (Figures 1,2 Table 1).
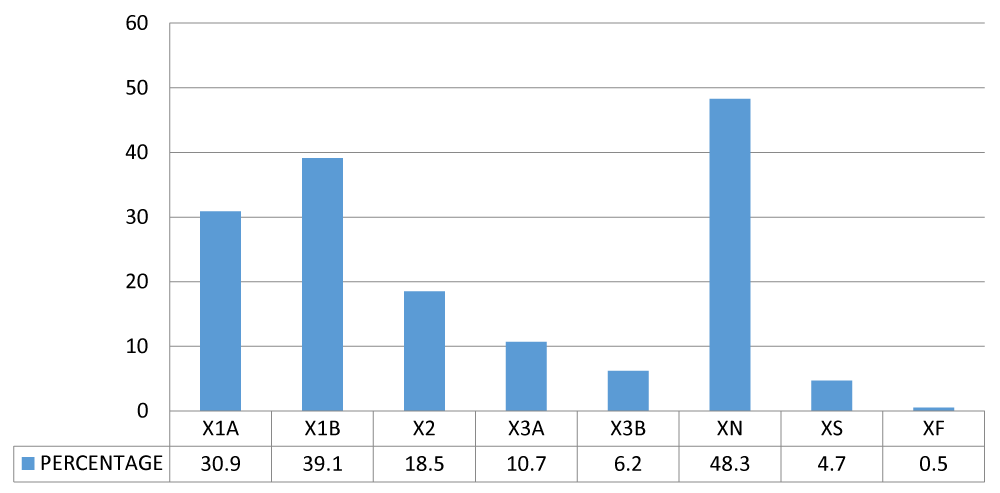
Figure 1: Bar chart showing percentage distribution of various grades of xerophthalmia in our study.
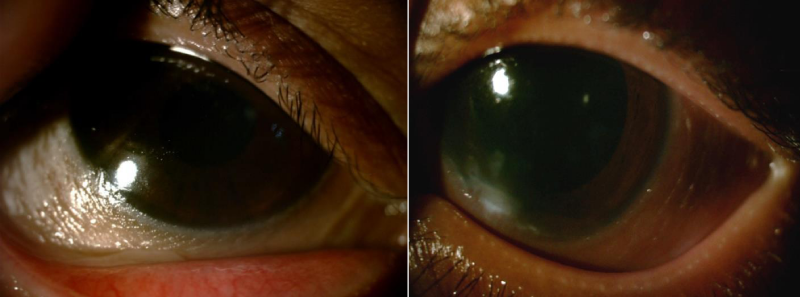
Figure 2: Child with bilateral bitot spot (right and left image) and corneal ulceration <1/3rd corneal surface left eye (right image).
| Table 1: Data showing prevalence of different grades of Xerophthalmia in our study. | ||
| Classification | No of Cases | Percentage |
| X1A---Conjunctival Xerosis | 912 | 30.9 |
| X1B---Bitot’s spots | 1154 | 39.1 |
| X2---Corneal Xerosis | 532 | 18.5 |
| X3A---Corneal Ulceration/Keratomalacia (<1/3 corneal surface) | 316 | 10.7 |
| X3B--- Corneal Ulceration/Keratomalacia (>1/3 corneal surface) | 184 | 6.2 |
| XN---Night Blindness | 1423 | 48.3 |
| XS---Corneal scar | 140 | 4.7 |
| XF--- Xerophthalmic Fundus | 16 | 0.5 |
Discussion
Vitamin A deficiency has been long recognized as a major cause of blindness and an important public health problem among children in India. The current study observed 4.43 % prevalence of xerophthalmia in children 2-6 years of age. The earlier-conducted studies have reported a prevalence of xerophthalmia in the range of 1.1 % to 22.3 % in different population groups and in different parts of the country [4-11].
The observed association between various the sociodemographic factors (lower socio-economic status, girl preponderance, more than one child of same family) and xerophthalmia was also endorsed by the results of previous studies [5,6]. Prevalence of night blindness, estimated to be 2.93 % is far above the minimum prevalence to determine its public health significance (1%), suggesting moderate degree of public health problem. A high prevalence of night blindness can serve as a mapping tool in developing targeted programmes, and as a method for the community to monitor its population’s vitamin A status, particularly in response to an intervention. Prevalence criteria for determining the public health significance of xerophthalmia and vitamin A deficiency in children aged 6 months to 6 years [12].
Indicator Minimum prevalence (%)
Night blindness (XN) >1
Bitot spots (X1B) >0.5
Corneal xerosis/corneal ulceration/keratomalacia (X2/X3A/X3B) >0.01
Corneal scar (XS) >0.05
Prevalence of night blindness to define a public health problem and its level of importance among children aged 24-71 months [13] .
Degree of public health problem, % Prevalence of night blindness
Mild 0.01-0.99
Moderate 1.0-4.9
Severe 5.0 or more
Efforts to reduce vitamin A deficiency in younger children to a level not considered to be of public health significance are encouraging but a challenging task remains in countries where the number of children affected is larger than previously expected. Organizations committed to eliminating vitamin A deficiency need to re-evaluate policies for reducing vitamin A deficiency in populations similar to those covered by the present study. Xeropthalmia is common in rice eating states in India e.g. Bihar, West Bengal, Tamil Nadu, Andhra Pradesh, Orissa, because rice is devoid of Carotene [14,15].
Conclusion
Vitamin A deficiency is recognized to be a severe public health problem leading to corneal opacity and childhood blindness in most of the areas of North India.
Health education is needed for dietary diversification to include vegetables and fruits for long-term sustainability in improving the vitamin A status of children of all age groups. Such an approach will improve the intake of vitamin A and other micronutrients in a balanced manner.
References
- Sommer A, West KP Jr. Vitamin A Deficiency: Health, Survival, and Vision. New York, Oxford University Press. 1996.
- Underwood BA, Arthur P. The contribution of vitamin A to public health. FASEB J. 1996; 10: 1040-1048. Ref.: https://goo.gl/5tKAu6
- Sherwin JC, Reacher MH, Dean WH, Ngondi J. Epidemiology of vitamin A deficiency and xerophthalmia in at-risk populations. Trans R Soc Trop Med Hyg. 2012; 106: 205-214. Ref.: https://goo.gl/khARNF
- Bahreynian M, Qorbani M, Naderimagham S, Nejatinamini S, Ataie-Jafari A. Burden of disease attributable to vitamin A deficiency in Iranian population aged less than five years: findings from the global burden of disease study 2010. J Diabetes Metab Disord. 2017; 16: 32. Ref.: https://goo.gl/ke1qfY
- Garg S, Nayar S, Garg A, Sane S. Vitamin A deficiency in preschool children. Indian Pediatrics. 1984; 21: 491-494. Ref.: https://goo.gl/2Dws5P
- Sharma SK, Mathur GP, Mathur S, Singh Y. An epidemiological study of hypovitaminosis a in preschool children of urban slums in Gorakhpur. Indian J Prev Soc Med. 1985; 16: 131-136.
- Katiyar GP, Jaiswal P, Reddy DCS, Agrawal, KN. Biosocial determinants of xerophthalmia in under-five children. Indian J Prev Soc Med. 1986; 17: 69-78.
- Kartha GP, Purohit CK. Prevalence of xerophthalmia-an evaluation in the context of ongoing National vitamin A supplementation program in five villages of Dholka Taluka of Ahmedabad District. Indian J Com Med. 1991; 16: 115-8.
- Sampathkumar V, Abel R. Xerophthalmia in rural South Indian children. Indian Pediatrics. 1993; 30: 246-248. Ref.: https://goo.gl/Y8LK1g
- Fakhir S, Srivastava I, Ahmad P, Husan SS. Prevalence of xerophthalmia in preschool children in an urban slum. Indian Pediatr. 1993; 30: 668-670. Ref.: https://goo.gl/8uRGzp
- Chamani N, Sharma P, Meena N, Sharma U. Pattern of vitamin deficiencies among the malnourished preschool children in ICDS blocks of Jaipur city. Indian J Matern Child Health. 1994; 5: 109-111. Ref.: https://goo.gl/2x2eaD
- Pal R, Sagar V. Antecedent risk factors of xerophthalmia among Indian rural preschool children. Eye Contact Lens. 2008; 34: 106-108. Ref.: https://goo.gl/JCjsjb
- Control of vitamin A deficiency and xerophthalmia. Report of a joint WHO/UNICEF/USAID/Helen Keller International/IVACG meeting. Geneva: World Health Organization. 1982. Ref.: https://goo.gl/5gqir2
- Indicators for assessing vitamin A deficiency and their application in monitoring and evaluation intervention programmes. Geneva: World Health Organization. 1996. Ref.: https://goo.gl/78RYoQ
- Prashant Bhushan, Deepak Mishra, Singh MK, Gyan Prakash Singh. Preventions and cures for xerophthalmia; a re-visit. Int J Cur Bio Med Sci. 2012; 2: 203-204.