Research Article
Outcome of Trabeculectomy in Advanced Glaucoma in a tertiary hospital in Rivers State, Nigeria

Awoyesuku EA* and Fiebai B
Department of Ophthalmology, University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria
*Address for Correspondence: Elizabeth A Awoyesuku, Department of Ophthalmology, University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria, Tel: +2348033088992; Email: [email protected]
Dates: Submitted: 11 December 2018; Approved: 18 December 2018; Published: 19 December 2018
How to cite this article: Awoyesuku EA, Fiebai B. Outcome of Trabeculectomy in Advanced Glaucoma in a tertiary hospital in Rivers State, Nigeria. Int J Clin Exp Ophthalmol. 2018; 2: 027-031. DOI: 10.29328/journal.ijceo.1001018
Copyright Licence: © 2018 Awoyesuku EA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Advanced glaucoma; Intra ocular pressure; Trabeculectomy; Visual acuity
Abstract
Aim: To evaluate the outcome of Trabeculectomy in advanced glaucoma in a hospital in Rivers State, Nigeria.
Methods: This was a non-randomized interventional study in which each patient served as its own control. Patients with advanced glaucoma and demonstrable field defects and Mean defect ≥-12 were included. The intervention employed was Trabeculectomy and IOP and visual acuity pre operative, as well as post op were collected and compared at pre- op, post -op day 1, one week, one month, 6 months. Data was analyzed using SPSS version 20.
Results: Thirteen (13) eyes from ten (10) patients with advanced glaucoma were involved in the study. Mean age of study population was 53±19.62 years. Mean of mean defect was -19.05±5.23dB while mean of vertical cup disc ratio (VCDR) was 0.88±0.04.
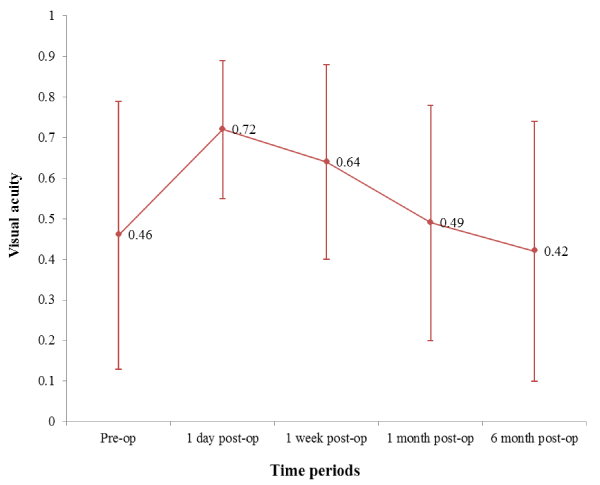
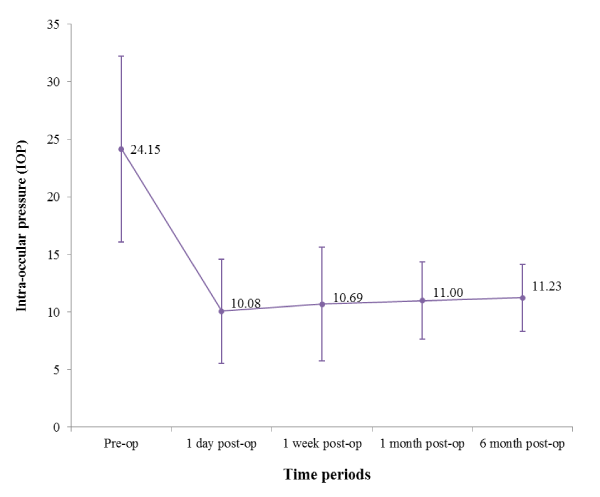
Mean of Pre- op Visual acuity (log MAR) was 0.46 and dropped to 0.72 first day post-op but improved over 6 months to 0.42. The mean of IOP pre-op was 24.15mmHg and dropped to 11.23mmHg (58.24%) over 6 months (p=0.001).
Conclusion: Trabeculectomy still remains the gold standard surgical treatment for glaucoma. In our study it resulted in a 58.24% drop in IOP over 6 months with mean visual acuity maintained at pre-op levels after 6 months follow up. It therefore is effective and safe surgical intervention in advanced glaucoma.
Introduction
Glaucoma remains the leading cause of irreversible blindness worldwide [1] and the second leading cause of blindness following cataract. The situation is not different in Nigeria with glaucoma accounting for a blindness prevalence of 0.7% in individuals 40years and above [2].
A large proportion of patients also present at an advanced stage of the disease and are often blind in one eye at time of presentation to the health facility [3-5].
Trabeculectomy remains the gold standard for surgical treatment and is widely used as a means of intraocular pressure control in glaucoma but rarely used in advanced glaucoma for fear of “wipe out” phenomenon, visual deterioration, hypotony and associated complications.
Materials and Methods
This was a non-randomized interventional study in which each patient served as its own control. Patients with advanced glaucoma and demonstrable field defects evaluated using Humphrey 750i perimeter (Carl Zeiss Meditec AG) with Mean defect ≥-12 were included. Slit lamp biomicroscopy with +78D Volk lens was done to assess optic disc characteristics and the vertical cup disc ratio corroborated with an optical coherence tomogram (Topcon 3D OCT- Maestro).Preoperatively, visual acuity using Snellens chart and intraocular pressure using Perkins hand held tonometer was assessed.
The intervention employed was Trabeculectomy done under local anaesthesia (sub conjunctival) using 2% Xylocaine + adrenaline over the supero- temporal quadrant. A superior fornix based peritomy was raised after injecting with 2% Xylocaine + adrenaline and bleeders cauterized using bipolar wet field cautery.
A superficial triangular sclera block was raised approximately 3mm by4mm and just before proceeding into clear cornea a cotton tip soaked with 0.2 mg/ml of Mitomycin C was applied under the conjunctiva for 2 minutes and thereafter rinsed thoroughly with 30 mls of normal saline. Dissection was continued into clear cornea using size 15 blade.
The anterior chamber was entered using a size 11 blade and deep sclera block removed with the help of a Kelley’s punch. A peripheral iridectomy was done and superficial sclera block is closed at the apex using a single 9/0 nylon suture while the conjunctiva is sutured with 8/0 Vicryl. Subconjunctival injection of 0.5ml of Gentamycin and 0.5ml of Dexamethasone was given, 0.25% Povidone iodine was instilled and eye pad applied for 24 hours.
On the first day post op, visual acuity and intra ocular pressure (IOP) was assessed while gutt Atropine 3 times daily, Prednisolone 2hourly, Ciprofloxacin 2hourly and 2.5% Povidone iodine nocte started.
IOP and visual acuity pre operative, as well as post op were collected and compared at pre- op, post -op day 1, one week, one month, 6 months. Data was analyzed using SPSS version 20.
Results
Thirteen (13) eyes from ten (10) patients with advanced glaucoma were involved in the study. Mean age of study population was 53±19.62 years. Median age was 57 years and age range was 25-79 years. M: F=1.5:1
Mean of mean defect was -19.05±5.23dB while mean of vertical cup disc ratio (VCDR) was 0.88±0.04.
Mean of Pre- op Visual acuity (log MAR) was 0.46 and worsened to 0.72 on first day post-op. It however improved over 6 months to 0.42.
The mean of Intra ocular pressure (IOP) pre-op was 24.15mmHg and dropped to 11.23mmHg (58.24%) over 6 months (p=0.001) (Tables 1-3)(Figures 1,2).
| Table 1: Comparison of mean age among males and females inthe study. | ||||
| Sex | ||||
| Variable | Male Mean± SD | Female Mean ±SD | t test | p-value |
| Age in years | 49.50±17.44 | 59.00±23.99 | -0.730 | 0.486 |
| SD – Standard deviation | ||||
| Table 2: Distribution of mean defect on SAP and mean VCDR of respondents | ||
| Variables | Mean ± SD | Median (range) |
| Defect on SAP | -19.05±5.23 | -21.08 (-11.66 – 27.16) |
| VCDR | 0.88±0.04 | 0.90 (0.80 – 0.90) |
| SD – Standard deviation | ||
| Table 3: Comparison of mean Visual acuity in males and females across the different time periods | ||||
| Male Visual Acuity |
Female Visual acuity |
|||
| Time periods | Mean ± SD | Mean ± SD | t test | p-value |
| Pre-op | 0.42±0.45 | 0.58±0.21 | -0.651 | 0.533 |
| 1 day post-op | 0.75±0.18 | 0.80±0.16 | -0.452 | 0.663 |
| 1 week post-op | 0.65±0.26 | 0.68±0.25 | -0.152 | 0.883 |
| 1 month post-op | 0.42±0.37 | 0.63±0.24 | -0.999 | 0.347 |
| 6 months post-op | 0.27±0.31 | 0.68±0.25 | -2.168 | 0.062 |
| SD – Standard deviation | ||||
Figure 1: Error bar chart showing mean visual acuity of respondents across the different time periods
Figure 2: Error bar chart showing mean IOP of respondents across the different time periods Friedman ANOVA= 23.392; p-value=0.001
Discussion
Trabeculectomy with Mitomycin C appears to be a safe and effective way to reduce intra ocular pressure in advanced glaucoma. It may however, be associated with visual acuity deterioration of one or 2 snellen lines.
Stead et al. [6], while studying outcome of Trabeculectomy in advanced glaucoma found a mean IOP of 11.3 to 13.3 over one to seven years follow up while a few patients had significant reduction in visual acuity of two or more Snellen lines. This correlates closely with our study with a mean IOP of 11.23mmHg, though our study did not corroborate severe impairment in visual acuity, indeed visual acuity improved slightly in our study after follow up for 6 months. The mean drop in intra ocular pressure in our study was statistically significant between pre op and 6 months post op, but, compared monthly it was not significant. The change in visual acuity was however not statistically significant.
A similar study in Nigeria by Anand et al. [7], with a follow up period of 6 months got a 30% reduction of IOP from baseline while VA decrease was less than 3 Snellen lines, this compares favorably with our study also. Baser et al. [8] in a retrospective study of 34 Trabeculectomies in advanced glaucoma, recorded a post op mean IOP of 14.8mmHg from a pre op mean of 28.4mmHg. Pre op mean visual acuity was 0.87(log MAR) and the mean defect on Standard automated Perimetry was -24.5. Inspite of the advanced stage of disease no patient experienced a wipe out. In our own study the mean of the mean defect was -19.05dB and no wipe out was reported.
Advanced visual field loss at diagnosis of glaucoma may be a major risk factor for blindness. In such patients, primary surgery is imperative to reverse this [9-11]. Surgery in advanced glaucoma is not without risks as permanent vision loss can be a consequence as reported by Francis et al. [12], where 8% of eyes operated had permanent vision loss.
Soatiana et al. [13], comparing outcomes of Trabeculectomies across Africa reviewed studies from 5 Sub Saharan countries. For these studies IOP control was successful with a range of 10-22mmHg (drop of 61.8-90%). Visual acuity remained unchanged in 30%, improved in 31-81% and worsened in 8.9-30.8% of patients studied. Studies done in Northern Nigeria [14,15], recorded 82- 97.4% IOP control (<21mmHg) after Trabeculectomy, while in Western Nigeria [16], IOP control was achieved in 70.7%. Thommy CP and Bhar IS [17] also studying Nigerian patients with advanced glaucoma had control of IOP in 95.4% with visual status remaining stable over follow up.
Despite the good control of IOP with Trabeculectomy and the minimal visual deterioration in patients even with advanced glaucoma, the practice of Trabeculectomy in glaucoma has fallen drastically. The advent of prostaglandin analogues and fear of surgical complications such as hypotony, shallow or flat anterior chamber, maculopathy, blebitis, endophthalmitis, “wipe out” amongst others associated with surgery has reduced both the practice / uptake of surgery.
Patients with advanced glaucoma are worse off as many surgeons will only do Trabeculectomy for early or moderately severe glaucoma. Kizor-Akariwe and Ogbonnaya CE [18], in a study of the practice of Trabeculectomy amongst Nigerian ophthalmologists found that only 57.1% had performed Trabeculectomy in the preceding year with a dismal Trabeculectomy rate of 0.9/ ophthalmologists/month.
Our study group is very small and this is a major limitation of our study. The study however still shows that surgery in advanced glaucoma can be relatively safe. We did not have any major vision threatening complications but the patients did complain of foreign body sensation, redness, and photophobia.
Conclusion
Trabeculectomy still remains the gold standard surgical treatment for glaucoma. In our study it resulted in a 58.24% drop in IOP over 6 months while mean visual acuity was maintained at near pre-op levels after 6 months follow up. It therefore is effective and safe surgical intervention in advanced glaucoma.
References
- Quigley HA. The number of people with glaucoma worldwide. Br J Ophthalmol. 1996; 80: 389-393. Ref.: https://goo.gl/qfe66M
- Abdul MM, Sivasubramaniam S, Murthy G, Gilbert C. Causes of blindness and visual impairment in Nigeria: the Nigerian blindness and visual impairment survey. Invest Ophthalmol & Vis Sci. 2009; 50: 4114-4120. Ref.: https://goo.gl/ST9V5n
- Awoyesuku EA, Ejimadu CS. Visual disability from Primary Open Angle Glaucoma (POAG) in University of Port Harcourt Teaching Hospital. Niger J Med. 2012; 21: 78-80. Ref.: https://goo.gl/R69Nfh
- Omoti AE, Osahon AI, Waziri-Erameh MJ. Pattern of presentation of primary open-angle glaucoma in Benin City, Nigeria. Tropical Doctor. 2006; 36: 97-100. Ref.: https://goo.gl/iDTwgS
- Dawodu OA, Osahon AI, Emifoniye E. Prevalence and causes of blindness in Otibhor Okhae Teaching Hospital, Irrua, Edo State, Nigeria. Ophthalmic Epidemiol. 2003; 10: 323-330. Ref.: https://goo.gl/QVY9ff
- Stead RE, King AJ. Outcome of Trabeculectomy with Mitomycin C in patients with advanced glaucoma. Br J Ophthalmol. 2011; 95: 960-965. Ref.: https://goo.gl/9CCjeC
- Anand N, Mielke C, Dawda VK. Trabeculectomy outcomes in advanced glaucoma in Nigeria. Eye (Lond) 2001; 15: 274-278. Ref.: https://goo.gl/nfYYQP
- Baser EF, Seymenoglu G, Mayali H. Trabeculectomies for advanced glaucoma. Int Ophthalmol. 2011; 31: 439-446. Ref.: https://goo.gl/7jYNT2
- King AJ, Fernie G, Azuara-Blanco A, Burr JM, Garway-Heath T, et al. Treatment of Advanced Glaucoma Study: a multicentre randomized controlled trail comparing primary medical treatment with primary Trabeculectomy for people with newly diagnosed advanced glaucoma-study protocol. Br J Ophthalmol. 2018; 102: 922-927. Ref.: https://goo.gl/jRxEjD
- Peters D, Bengtsson B, Heijl A. Factors associated with lifetime risk of open-angle glaucoma blindness. Acta Ophthalmol. 2014; 92: 421-425. Ref.: https://goo.gl/mw2cGv
- Anthony King, Augusto Azuara-Blanco, Anja Tuulonen. Clinical Review Glaucoma. BMJ 2013; 346: f3518. Ref.: https://goo.gl/uNDV9g
- Francis BA, Hong B, Winarko J, Kawji S, Dustin L, et al. Vision loss and Recovery after Trabeculectomy, risk and associated risk factors. Arch Ophthalmol. 2011; 129: 1011-1017 Ref.: https://goo.gl/jHhjNh
- Soatiana JE, Kpoghoumou MA, Kalembo FW, Zhen HH. Outcomes of Trabeculectomy in Africa. Open Journal of Ophthalmology; 2013; 3: 76-86. Ref.: https://goo.gl/gwpcC3
- Ndife TI, Abdullahi SM, Raji L, Umar MM, Olaniyi S, et al. Long-term outcome of Trabeculectomy with and without small incision cataract surgery at a tertiary eye hospital in Northern Nigeria. Niger J Ophthalmol. 2017; 25: 110-113 Ref.: https://goo.gl/8T5inQ
- A Lawan. Pattern of presentation and outcome of surgical management of primary open angle glaucoma in Kano, Northern Nigeria. Ann Afr Med. 2007; 6: 180-185. Ref.: https://goo.gl/CSBBME
- Adegbehingbe BO, Majemgbasan T. A review of Trabeculectomies at a Nigerian Teaching Hospital. Ghana Med J. 2007; 41: 176-180. Ref.: https://goo.gl/EV5opZ
- Thommy CP, Bhar IS. Trabeculectomy in Nigerian patients with open angle glaucoma. Br J Ophthalmol. 1979; 63: 636-642. Ref.: https://goo.gl/w2kHBi
- Kizor- Akaraiwe NN, Ogbonnaya CE. Practice of Trabeculectomy by Ophthalmologists in Nigeria. Niger J Clin Pract. 2017; 20: 507-511. Ref.: https://goo.gl/a6y3BY