Review Article
Alternative treatment methods in eyes with pseudophakic cystoid macular edema

Ayse Gul Kocak Altintas*
Saglik Bilimleri University, Ulucanlar Eye Hospital, Ankara, Turkey
*Address for Correspondence:Ayse Gul Kocak Altintas, Saglik Bilimleri University, Ulucanlar Eye Hospital, Ankara, Turkey, Tel: +90 532 798 84 88; Email: [email protected]
Dates: Submitted: 21 December 2019; Approved: 02 January 2019; Published: 03 January 2019
How to cite this article: Altintas AGK. Alternative treatment methods in eyes with pseudophakic cystoid macular edema. Int J Clin Exp Ophthalmol. 2019; 3: 001-007. DOI: 10.29328/journal.ijceo.1001019
Copyright Licence: © 2019 Altintas AGK. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pseudophakic cystoid macular edema; Irvine-Gass syndrome; Steroid; Non-steroidal anti-inflammatory drugs; Ozurdex; Anti- Vascular endothelial growth factors
Abstract
Cystoid macular edema is a common cause for unexplained painless vision loss after cataract surgery. Even the pathogenesis of pseudophakic cystoid macular edema (PCME) still remains undefined, it can most frequently occur in eyes with high vasoactive profile, had complicated cataract surgery such as posterior capsule rupture and risk of inflammation. Increased inflammation, ultimately leading to the breakdown of the blood-retinal barrier and cystic accumulation of extracellular intraretinal fluid. The natural history of PCME is spontaneous resolution without any treatment in most of patient, but it may take weeks or months, in addition permanent visual morbidity may occur in some cases. Therefore there is lack of consensus regarding treatment approach for this common ocular condition.
In this review treatment alternatives of PCME and its relation with underlying patho-physiologic mechanism are evaluated.
Introduction
Pseudophakic cystoid macular edema (PCME) also known as Irvine-Gass syndrome (IGS), was initially reported by Irvine in 1953. Gass and Norton subsequently reported its characteristics with fluorescein angiography [1-4]. IGS remains an important cause of painless decrease in vision following cataract extraction and intraocular lens (IOL) implantation. IGS is most frequently occurs in patients had glaucoma treated with prostaglandin drops and posterior capsule ruptured eye during the cataract surgery. This syndrome is present in around 4–12 weeks after cataract surgery and often resolves spontaneously in 70-90 % of the cases; which can takes from 2 months to a year. Epidemiological studies show that, 50% of these cases have resolution within 6 months after surgery, and 90% of them in 2 years [3-7].
Patho-physiologic mechanism
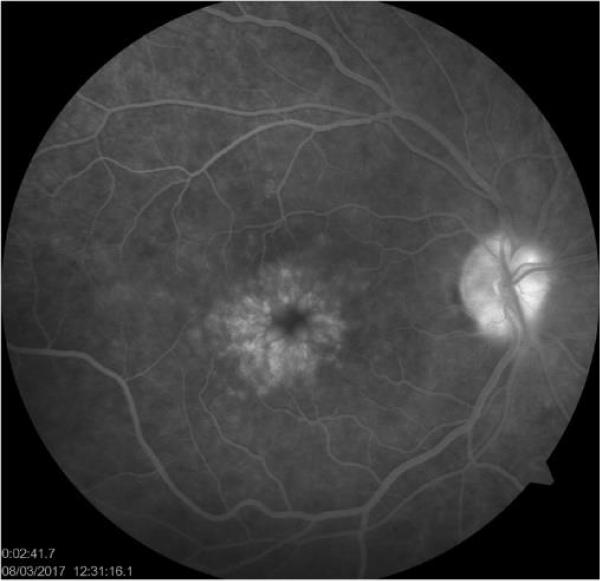
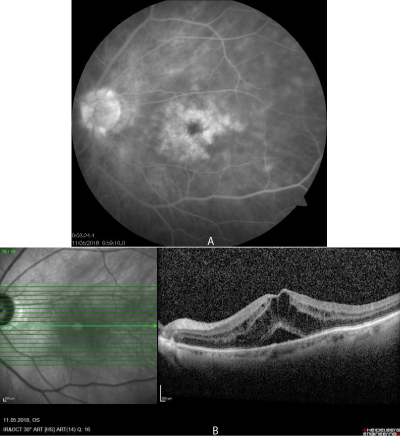
The patho-physiologic mechanism for IGS is multifactorial including excessive surgical trauma increased inflammation, posterior capsule rupture, evitreous disturbance, hypotony. Surgical trauma triggers the cascade of inflammatory reactions, leading to conversion of arachidonic acid to prostacyclins, prostaglandins thromboxanes, leukotriens and other inflammatory mediators. These inflammatory mediators cause the breakdown of the blood–retinal barrier that ultimately increased retinal capillary permeability and extracellular fluid accumulation mainly in the outer plexiform and inner nuclear layers characterized by petalloid perifoveal leakage on fluorescent angiography (FA). Hyperfluorescens of optic nerve head on the later stage of FA without retinal hemorrhage, vascular torsisity and exudates are the important sings of PCME (Figure 1). Increased macular thickness with cystoid empty spaces, corresponding to petalloid leakage on FA, in optical coherent tomography (OCT) is one of the significant finding of postoperative CME (Figure 2a,b) Increased prostaglandins within the eye also cause vasodilation and leukocyte migration. With these process, Müller cells become swollen and lysed than eventually developed cystic changes that result in varying degree of decrease in visual acuity. This detrimental effect on visual acuity may occasionally persist and lead to permanent vision loss [3,5,7-9].
Figure 1: Petalloid perifoveal leakage and hyperflourescence of optic nerve on fluorescein angiography (FA)
Figure 2: Macular petalloid leakage and optic nerve head hyperflourescens on fluorescein angiography in eyes with Irvine Gass syndrome. b: Cystic macular edema in the same eye of the same patient evaluated by OCT in the same day.
Prophylaxis and treatment
Prophylaxis: Prophylaxis is recommended mainly for patients who have the risks of developing cystoid macular edema after cataract surgery, such as patients with diabetes, retinal vein occlusion, uveitis and patients with glaucoma treated by topical prostaglandin eye drops. The incidence of IGS has been reported 0.1- 5% according to different reports, Several meta-analyses and systematic reviews have reported that a significant reduction in incidence of CME after cataract surgery with prophylactic use of topical nonsteroidal anti-inflammatory drugs (NSAID), including ketorolac 0.4%, bromfenac 0.1%, nepafenac 0.1% and diclofenac 0.1%. Topically applied NSAIDs reduce prostaglandin synthesis by inhibiting the cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) enzymes [10-14]. Topical anti-glaucoma treatment rather than prostaglandin at least one week before surgery can reduced the risk of PCME development.
In systematic reviews and meta-analysis of randomized controlled trials have reported the effects of prophylactic topical NSAIDs; either as monotherapy or combined with topical corticosteroids, appear to be more effective than topical corticosteroids such as betamethasone, fluorometholone, dexamethasone or prednisolone asetonide alone to reduce the risk of developing PCME within 3 months after surgery. Similarly, results of controlled trials showed that the prevalence of CME 1 month after surgery was significantly lower among patients treated with NSAIDs (3.8%) comparing to patients treated with either potent or weaker corticosteroids (25.3%) [12-17].
Treatment alternatives
There is no standardized treatment protocol for Irvine-Gass syndrome due its multifactorial pathogenesis and spontaneous resolution in most of the cases. Spontaneous resolution without any treatment, may take weeks or months, so for patients, especially those who have vision-dependent occupations and live active lifestyles, treatment should start as early as possible [10-13].
Topical nsaid treatment
A number of meta-analyses and systematic reviews have reported several treatment alternatives included, topical NSAIDs and steroids application, intravitreally or sub-Tenon's injections of triamcinolone acetonide, intravitreally Anti-VEGF injections, oral carbonic anhydrase inhibitors, immunomodulators therapy and in cases secondary to vitreous traction, other surgical approaches such as Nd: Yag laser vitreolysis, vitrectomy [9,12,13].
The most frequently applied treatment choice include aggressive topical steroids, with or without NSAIDs, aimed at minimizing inflammation. Even in an analysis of several placebo-controlled trials, macular edema was reported in 0.7% in eyes receiving bromfenac 0.09% while 1.4% of patients receiving placebo, the benefits of topical NSAIDs in treating PCME are not well demonstrated comparing to their prophylactic effects. In addition combination therapy with corticosteroids and topical NSAIDs significantly more effective than corticosteroids alone in treating IGS [12-16].
Corticosteroid treatment
Administration of corticosteroids through various routes, other than topical application have been used for several years mostly. But still there is a little consensus on the efficacy of various therapeutic options such as, peribulbar, retrobulbar, or intravitreal in patient with foveal thickness more than 250 μm lasting for at least 90 days after the initiation of topical treatment [16-18].
Randazzo et al. [19], reported a significant decreased in foveal thickness after 0.8 cc of 4 mg betamethasone sub-Tenon injections. They also observed reduction in metamorphopsia and improved color sensitivity with this treatment.
The sub-Tenon route is considered equal to the retrobulbar route in terms of efficacy, but the sub-Tenon route is generally considered safer with respect to IOP elevation. On the other hand result of several studies showed a significant IOP rise with the use of triamcinolone acetonide (TA) that did not correlate with the route of application. According to most of reports in the literature, there is a common opinion about a higher incidence of IOP elevation beyond 30 mm Hg following intravitreal triamcinolone acetonide (IVTA) injection which has higher intravitreal concentration compared to peribulbar injection [17-19].
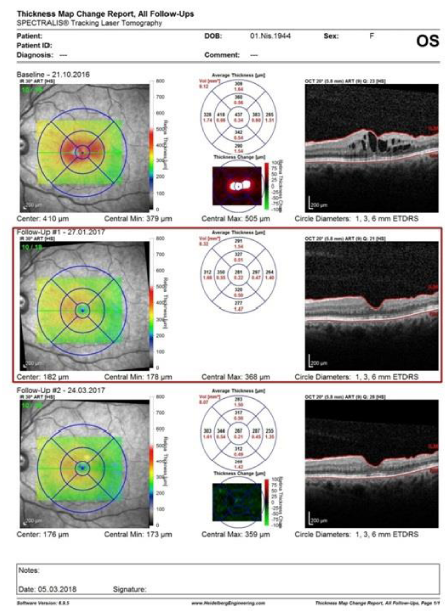
Dexamethasone as another corticosteroid has a 6-fold more potent anti-inflammatory effect than TA. One of the other disadvantages of IVTA is the transient therapeutic effect necessitating repeated injections. Sustained-release dexamethasone implant (Ozurdex) (Allergan, Inc.) have been developed to overcome this problem which sustained steroid levels and biological activity for 6 months, with peak levels of drug remains in the first 3 months [20-24]. This biodegradable systems made of poly lactic acid-co-glycolic acid (PLGA) matrix material which dissolves completely in the vitreous and provides sustained release of 0.7 mg of preservative-free dexamethasone during 6 months period (Figure 3) [20-22].
Figure 3: Differential map between the first and the last OCTs showed a foveal thickness reduction after treatment with dexamethasone implant (Ozurdex).
Williams et al. [21] observed a considerable improvement in BCVA from 0.3 lines pre-Ozurdex injection to 0.8 lines post-Ozurdex injection. Similarly Mayer et al. [22] reported that the mean VA increased from 30.2 letters at baseline to 50.4 with the ozurdex treatment while the foveal thickness decreased from 520.8 ± 71.4 μm to 232.7 ± 26.6 μm at 12 months. Landré et al. [23], reported a significant improvemed in term of macular edema treatment in which the mean central foveal thickness decreased from 598 μm. to 286 μm at month 1, 338 μm at month 3, and was 441 μm at month 12 with Ozurdex injection. They reported that some of their patients needed another dexamethasone implant injections. Klamann et al. [24] reported that 66% of their patient out of 12 patients needed more than one injection and recurring macular edema had been completely reduced by repeated injections.
Bellocq [25], reported that even 49% of 50 patient received a second Ozurdex injection and by this treatment neither functional nor anatomical recurrence was observed at least 1 year followed-up. They reported a significant decrement in macular thickness which was 544±117.2 μm before treatment and decreased to 302 μm and 61.2% of patients had an increase of more than 15 letters with the Ozurdex treatment. A good anatomic and functional response and safety patterns were similar in each injection which demonstrating Ozurdex's reproducibility.
Altintas et al. [26] reported a significant reduction in macular thickness with a single Ozudex implantation from 733 u to 197 u in eyes with unresponsive to intravitreal Anti-VEGF who is using inhaler steroid. This report showed that PCME can be developed even under systemic steroid treatment and intravitreal Ozudex implantation can be effective in such a difficult patient.
The intravitreal dexamethasone implant promising alternative therapy to achieve rapid resolution in recalcitrant post-surgical cystoid macular edema, refractory to topical treatments. It has a relatively better safety profile, reduce complications with low recurrence rate [27-29].
Anti-vascular endothelial growth factors (Vegf)
Despite the treatment options for IGS include NSAID and corticosteroids new fields of clinical research including the use of anti-vascular growth factors considered a good therapeutic choice [30].
Vascular endothelial growth factors (VEGF) are inflammatory mediators which induce vascular permeability by their indirect effect on vascular endothelial cells. They have a beneficial effect on the macular architecture, in the onset of macular edema because the inflammation is the major etiologic factor in the development of IGS. Successful treatment of IGS with intravitreal injection of either 1 mg or 1.25 mg bevacizumab (Avastin), a monoclonal antibody against all VEGF isoforms have been reported [30-32].
According to Mitropoulos et al. [33] report, single injection of Anti-VEGF was sufficient for the resolution of ME, while recurrence was observed in 1 patient out of 7 eyes.
Demirel et al. [34] reported a significant reduction in CMT after Intravitreal (0.5 mg/0.05 mL) ranibizumab injection in 2 eyes. Mason et al. [35], reported 2 patients with persistent IGS who had nearly immediate improvement of visual acuity 4 to 5 lines and a complete resolution of ME after a single intravitreal injection of 1.0 mg bevacizumab without further treatment. In contrast to this promising success rate Spitzer et al. [36] ,reported that visual functional improvement did not observed in most eyes with neither single nor repeated injection of bevacizumab at least when the drug is used as a mono- therapy. They reported that, eye received repeated injections had fluctuating levels of central retinal thickness, significantly lower thickness was observed after each injection but it increased again 6 to 10 weeks later.
Result of these clinical outcomes intravitreal ranibizumab and bevacizumab have been shown to be effective in some, but not all cases.
Other treatment choice
Mineralocorticoid receptor antagonists and spironolactone therapy, have been reported by Matet and coworkers [37], as an efficient combination with topical dexamethasone in refractory cases following complex cataract or retinal detachment surgery.
IFN alpha-2a at a dose of 3 million IU/day subcutaneously for 4 weeks has been demonstrated to be a successful treatment option for resistant chronic PCME in without any systemic or local side effects [38]. But it can be prefer only if other alternative methods are ineffective for treatment of PCME (Table 1).
| Table 1: Alternative medication in treatment of eyes with pseudophakic cystoid macular edema. | ||
| Non-Steroidal Anti-inflammatory Drugs (NSAID) | Topical | Ketorolac |
| Bromfenac | ||
| Nepafenac | ||
| Diclofenac | ||
| Steroids | Topical | Betamethasone |
| Fluorometholone | ||
| Dexamethasone | ||
| Prednisolone asetonide | ||
| Subtenon Pribulber Retrobulber |
Betamethasone | |
| Dexamethasone | ||
| Triamcinolone acetonide | ||
| Intravitreal | Dexamethasone | |
| Triamcinolone acetonide | ||
| Systemic | Minerelocrticosteroids | |
| Anti-Vascular endothelial growth factors (VEGF) | Intravitreal | Ranibizumab |
| Bevacizumab | ||
| Cytokine | Subcutaneously | Interferon alpha-2a |
Vitrectomy with removal of epiretinal membrane should be considered as a treatment modality in eyes had vitreomacular traction since tractional component may have adverse effect on the pathogenesis of PCME [39].
Long-lasting, recalcitrant postoperative macular edema is a therapeutic challenge therefore early diagnose and optimal treatment regimens will help to gain visual functions and prevent persistent visual disturbance.
References
- Yonekawa Y, Kim IK. Pseudophakic cystoid macular edema. Curr Opin Ophthalmol. 2012; 23: 26–32. Ref.: https://goo.gl/Cspwmg
- Daien V, Papinaud L, Domerg C, Lacombe S, Daures JP, et al. Incidence and characteristics of cystoid macular edema after cataract surgery. Ophthalmology. 2016; 123: 663–664. Ref.: https://goo.gl/hDfbEb
- Altıntaş AGK, Coban P, Arifoğlu HB, Koklu G, Ozcan PY, et al. Comparison of phaco parameters effect on macular thickness changes after uneventful phacosurgery in diabetic and non-diabetic patients. Int Eye Sci 2016; 16: 201-206. Ref.: https://goo.gl/16c9r4
- Packer M, Lowe J, Fine H. Incidence of acute postoperative cystoid macular edema in clinical practice. J Cataract Refract Surg. 2012; 38: 2108–2111. Ref.: https://goo.gl/zPXwEN
- Henderson BA, Kim JY, Ament CS, Ferrufino-Ponce ZK, Grabowska A, et al. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg. 2007; 33: 1550–1558 . Ref.: https://goo.gl/vvTRp5
- Zur D, Loewenstein A. Postsurgical cystoid macular edema. Dev Ophthalmol. 2010; 47: 148–159. Ref.: https://goo.gl/adVGCG
- Lobo C. Pseudophakic cystoid macular edema. Ophthalmologica. 2012; 227: 61–67. Ref.: https://goo.gl/qz5tjn
- Shields MK, Adler PA, Fuzzard DRW, Chalasani R, Teong JMY. A Case of Acute Bilateral Irvine-Gass Syndrome following Uncomplicated Phacoemulsification, Demonstrated with Optical Coherence Tomography. Case Rep Ophthalmol. 2015; 6: 143–148. Ref.: https://goo.gl/zaonTU
- Kiernan DF, Hariprasad SM. Controversies in the Management of Irvine-Gass Syndrome Ophthalmic Surgery, Lasers and Imaging Retina 2013; 44: 522-527. Ref.: https://goo.gl/mtTx2X
- Quintana NE, Allocco AR, Ponce JA, Magurno MG. Non steroidal anti-inflammatory drugs in the prevention of cystoid macular edema after uneventful cataract surgery. Clin Ophthalmol. 2014; 8: 1209–1212 . Ref.: https://goo.gl/4MnDaV
- Sheppard JD. Topical bromfenac for prevention and treatment of cystoid macular edema following cataract surgery: a review. Clin Ophthalmol. 2016; 10: 2099–2111. Ref.: https://goo.gl/kr2PsP
- Sahu S, Ram J, Bansal R, Pandav SS, Gupta A. Effect of topical ketorolac 0.4%, nepafenac 0.1%, and bromfenac 0.009% on postoperative inflammation using laser flare photometry in patients having phacoemulsification. J Cataract Refract Surg. 2015; 41: 2043–2048. Ref.: https://goo.gl/vxFdd1
- Walters TR, Goldberg DF, Peace JH, Gow JA, Bromfenac Ophthalmic Solution 0.07% Once Daily Study Group Bromfenac ophthalmic solution 0.07% dosed once daily for cataract surgery: results of 2 randomized controlled trials. Ophthalmology. 2014; 121: 25–33. Ref.: https://goo.gl/huAoTz
- Wittpenn JR1, Silverstein S, Heier J, Kenyon KR, Hunkeler JD, et al. A randomized, masked comparison of topical ketorolac 0.4% plus steroid vs steroid alone in low-risk cataract surgery patients. Am J Ophthalmol. 2008; 146: 554–560. Ref.: https://goo.gl/qZnny2
- Dal D, Sarac O, Toklu Y, Kocak Altintas AG, Cakmak HB, et al. The Effect of Perioperative Topical Ketorolac 0.5% on Macular Thickness after Uneventful Phacoemulsification. J Ophthalmol. 2017 ;2017: 4271671 . Ref.: https://goo.gl/kjniWk
- Warren KA Bahrani H Fox JE. NSAIDs in combination therapy for the treatment of chronic pseudophakic cystoid macular edema. Retina. 2010; 30: 260–266. Ref.: https://goo.gl/e3maK4
- Sivaprasad S McCluskey P Lightman S. Intravitreal steroids in the management of macular oedema. Acta Ophthalmol Scand. 2006; 84: 722–733. Ref.: https://goo.gl/rxoe6u
- Benhamou N1, Massin P, Haouchine B, Audren F, Tadayoni R, et al. Intravitreal triamcinolone for refractory pseudophakic macular edema. Am J Ophthalmol. 2003; 135: 246–249. Ref.: https://goo.gl/3JrZVo
- Randazzo A, Vinciguerra P. Chronic macular edema medical treatment in Irvine-Gass syndrome: case report. Eur J Ophthalmol 2010; 20: 462-465. Ref.: https://goo.gl/UYzSZp
- Herrero-Vanell R, Cardillo JA, Kuppermann BD. Clinical applications for the sustained-release dexamethasone implant for treatment of macular edema. Clin Ophthalmol. 2011; 5: 139–146. Ref.: https://goo.gl/9ddAoP
- Williams GA1, Haller JA, Kuppermann BD, Blumenkranz MS, Weinberg DV, et al. Dexamethasone posterior-segment drug delivery system in the treatment of macular edema resulting from uveitis or Irvine-Gass syndrome. Am J Ophthalmol. 2009; 147: 1048–1054. Ref.: https://goo.gl/4DQjiJ
- Mayer WJ, Kurz S, Wolf A, Kook D, Kreutzer T, et al. Dexamethasone implant as an effective treatment option for macular edema due to Irvine-Gasssyndrome. J Cataract Refract Surg. 2015; 41: 1954-1961. Ref.: https://goo.gl/xL8XH2
- Landré C, Zourdani A, Gastaud P, Baillif S. Treatment of postoperative cystoid macular edema (Irvine-Gass syndrome) with dexamethasone 0.7 mg intravitreal implant. J Fr Ophtalmol 2016; 39: 5-11. Ref.: https://goo.gl/hHNxQS
- Klamann A, Böttcher K, Ackermann P, Geerling G, Schargus M, et al. Intravitreal Dexamethasone Implant for the Treatment of Postoperative Macular Edema. Ophthalmologica. 2016; 236: 181-185. Ref.: https://goo.gl/UUVzBP
- Bellocq D, Korobelnik JF, Burillon C, Voirin N, Dot C, et al. Effectiveness and safety of dexamethasone implants for post-surgical macular oedema including Irvine-Gass syndrome: the EPISODIC stud study. Br J Ophthalmol 2015; 99: 979-983. Ref.: https://goo.gl/WHfNTD
- Altintas AGK, Ilhan C, Citirik M. The management of Irvine-Gass Syndrome in a patient using Inhaler steroid. Int J Clin Exp Ophthalmol. 2019; 2: 1-5. Ref.: https://goo.gl/sF1ViW
- Dutra Medeiros M1, Navarro R, Garcia-Arumí J, Mateo C, Corcóstegui B. Dexamethasone Intravitreal Implant for Treatment of Patients With Recalcitrant Macular Edema Resulting From Irvine-Gass Syndrome Investigative Ophthalmology & Visual Science. 2013; 54: 3320-3324. Ref.: https://goo.gl/LRyo6G
- Keilani C, Halalchi A, Wakpi Djeugue D, Regis A, Abada S. Evaluation of best corrected visual acuity and central macular thickness after intravitreal dexamethasone implant injections in patients with Irvine-Gass syndrome: A retrospective study of six cases. Therapie. 2016; 71: 457-465. Ref.: https://goo.gl/bbjHMD
- Sudhalkar A, Chhablani J, Vasavada A, Bhojwani D, Vasavada V, et al. Intravitreal dexamethasone implant for recurrent cystoid macular edema due to Irvine-Gasssyndrome: a prospective case series. Eye (Lond). 2016; 30: 1549-1557. Ref.: https://goo.gl/4NDvZa
- Fenicia V, Balestrieri M, Perdicchi A, Maurizi Enrici M, DelleFave M, et al. Intravitreal Injection of Dexamethasone Implant and Ranibizumab in Cystoid Macular Edema in the Course of Irvine-Gass Syndrome. Case Rep Ophthalmol. 2014; 5: 243–248. Ref.: https://goo.gl/ech1G1
- Arevalo JF1, Maia M, Garcia-Amaris RA, Roca JA, Sanchez JG, et al. Intravitreal bevacizumab for refractory pseudophakic cystoid macular edema: the Pan-American Collaborative Retina Study Group results. Ophthalmology. 2009; 116: 1481–1487. Ref.: https://goo.gl/8ikaQq
- Mason JO, Albert MA, Vail R. Intravitreal bevacizumab (Avastin) for refractory pseudophakic cystoid macular edema. Retina 2006; 26: 356-357. Ref.: https://goo.gl/nz1bsf
- Mitropoulos PG, Chatziralli IP, Peponis VG, Drakos E, Parikakis EA. Intravitreal Ranibizumab for the Treatment of Irvine-Gass Syndrome. Ocul Immunol Inflamm. 2015; 23: 225-231. Ref.: https://goo.gl/d9mJfs
- Demirel S, Batioğlu F, Özmert E. Intravitreal Ranibizumab for the Treatment of Cystoid Macular Edema in Irvine-Gass Syndrome. J Ocul Pharmacol Ther. 2012; 28: 636-639. https://goo.gl/fa4dtw
- Mason JO, III, Albert MA, Jr, Vail R. Intravitreal bevacizumab (Avastin) for refractory pseudophakic cystoid macular edema. Retina. 2006; 26: 356–357. Ref.: https://goo.gl/HC71a3
- Spitzer MS1, Ziemssen F, Yoeruek E, Petermeier K, Aisenbrey S, et al. Efficacy of intravitreal bevacizumab in treating postoperative pseudophakic cystoid macular edema. J Cataract Refract Surg 2008; 34: 70–75. Ref.: https://goo.gl/zLmA5N
- Matet A, Daruich A, Behar-Cohen F. Irvine-Gass Macular Edema Responding to the Combination of Oral Mineralocorticoid-Receptor Antagonist With Dexamethasone Drops. Ophthalmic Surg Lasers Imaging Retina. 2017; 48: 936-942. Ref.: https://goo.gl/WmUvbE
- Deuter CM1, Gelisken F, Stübiger N, Zierhut M, Doycheva D. Successful treatment of chronic pseudophakic macular edema (Irvine-Gass syndrome) with interferon alpha: a report of three cases. Ocul Immunol Inflamm. 2011; 19: 216–218. Ref.: https://goo.gl/QHBtyT
- Scarpa G. Bilateral cystoid macular edema after cataract surgery resolved by vitrectomy. Eur J Ophthalmol. 2011; 21: 677–679. Ref.: https://goo.gl/4evXba