More Information
Submitted: November 06, 2022 | Approved: November 21, 2022 | Published: November 22, 2022
How to cite this article: Srinivasan G, Madhumitha PS, Divya N. A retrospective observational study of mycotic keratitis in Saveetha Hospitals, Chennai. Int J Clin Exp Ophthalmol. 2022; 6: 038-044.
DOI: 10.29328/journal.ijceo.1001049
Copyright Licence: © 2022 Srinivasan G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A retrospective observational study of mycotic keratitis in Saveetha Hospitals, Chennai
Srinivasan G1, PS Madhumitha1 and Divya N3*
1Associate Professor, Department of Ophthalmology, Saveetha Medical College and Hospitals, Chennai, India
2Junior Resident, Department of Ophthalmology, Saveetha Medical College and Hospitals, Chennai, India
3Associate Professor, Department of Ophthalmology, Saveetha Medical College and Hospitals, Chennai, India
*Address for Correspondence: Dr. Divya N, Associate Professor, Department of Ophthalmology, Saveetha Medical College and Hospitals, Chennai, India, Email: [email protected]
Aim and objective:
1. To study the manifestations of fungal corneal ulcer in different age groups and sex
2. To study the distribution of fungal corneal ulcer in relation to occupation
3. To know the effect of Natamycin and Fluconazole as anti-fungal agents.
Materials and methods: This is a retrospective analysis of microbiology records of patients presenting with suspected microbial keratitis seen between January 2021 and June 2021. Patients with positive fungal cultures were analyzed in detail for the type of fungus isolated.
Results: 90 patients with suspected microbial keratitis were reviewed. A microbiological diagnosis of mycotic keratitis was established 9 (10%) patients over a period of 6 months, based on positive fungal cultures. Filamentous fungi were isolated more often than yeasts. Aspergillus species followed by Fusarium species were the commonest filamentous fungi isolated.
Conclusion: Over a period of 6 months, the cumulative incidence of mycotic keratitis was 10%. The pathogenic organisms most frequently responsible for mycotic keratitis were Aspergillus species. When beginning an empirical therapy for mycotic keratitis, etiological factors were helpful. Eight of the 90 patients with corneal ulcers who were admitted to the patient department for treatment had positive fungal cultures in Sabouraud’s media. The age range of 50 to 60 years had a high prevalence of illness.
There were 90 total cases of corneal ulcers. Out of those there were 8 (8.8%) incidences of fungal ulcers. More men than women were impacted. Workers in agriculture are more impacted than others.
The main cause of a fungus-induced corneal ulcer was trauma.
Natamycin was the better option for the treatment of fungal keratitis. Filamentous fungi (Aspergillus species, fusarium, and curvularia) responded effectively to Natamycin 5% eyedrop.
Slower therapeutic response, delayed diagnosis, and worse visual results are common characteristics of fungal keratitis [1-7]. Geographically speaking, the harmful organisms differ, with yeast being more prevalent in temperate climes while Fusarium and Aspergillus are more prevalent in tropical latitudes [8-12]. The key to an early diagnosis is clinical suspicion, especially in regions where fungi infections are relatively uncommon [13,14], Natamycin, voriconazole and amphotericin B are topical medications used to treat fungal keratitis [15]. With trials showing greater results in patients with filamentous fungus, natamycin is regarded as a first-line treatment for fungal keratitis [16,17]. In this retrospective study, we assessed the microbiologic traits, therapeutic approaches, and prognosis of patients who underwent treatment at our tertiary care academic medical centre for fungal keratitis, as determined by culture.
Saveetha Medical College’s department of ophthalmology conducted this study on mycotic keratitis from January to June of 2021. The outpatient department saw a total of 800 patients, of whom 90 cases (11.25%) of microbial keratitis and 8 cases (8.8%) of keratomycosis were observed. Upper eyelids were everted to exclude foreign body.
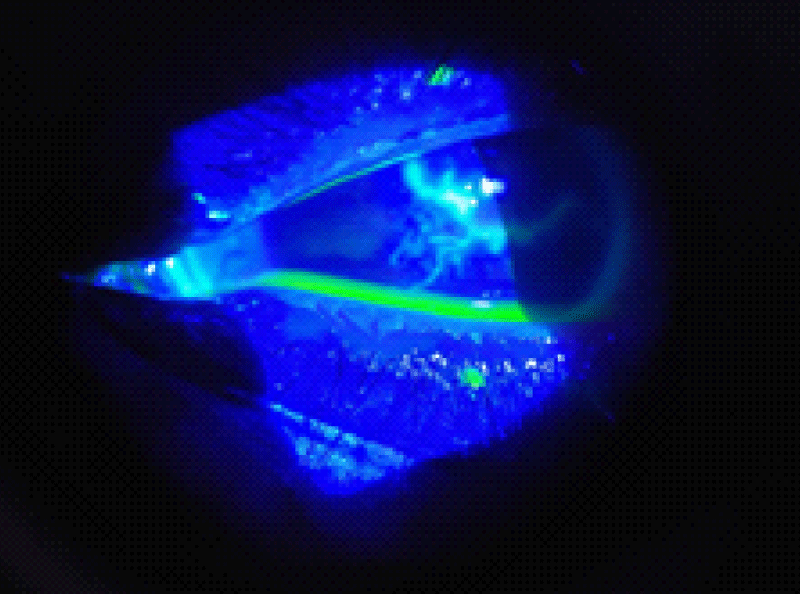
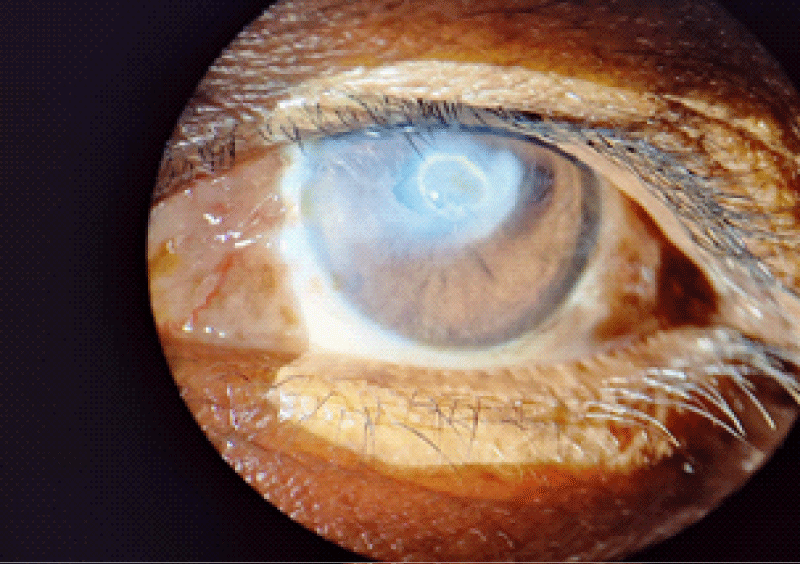
Size and depth of the lesions were measured and examined for satellite lesions (Figures 1,2). Prerequisites were: to numb the cornea, topical 4% lignocaine GeL, sterile universal speculum is used to split and fix the lids and to get a clear view of an ulcerated cornea it also guards against contamination from the conjunctiva and lid edge, to remove the ulcer, a disposable no. 15 bard parker scalpel blade was employed, glass slides measuring 10 cm × 4 cm × 0.2 cm, gram’s staining products, 10% KOH -related preparatory materials, sterile culture swipes for specimen collection [18]. On Blood sugar and chocolate agar for Aerobic organism, Thiogloycolate broth for Anaerobic organisms, and on Saboraud’S agar for fungi [19].
Figure 1: Fluorescein staining showing epithelial erosion.
Figure 2: Satellite lesion with white feathery irregular margins.
Methods
- Applying one drop of 4% Xylocaine every 1ml for 5 - 10 minutes will anaesthetize the cornea.
- Using a sterile universal speculum, expose the cornea.
- Scraping the cornea: The ulcer's exudate and necrotic debris are taken out. The corneal ulcer base and margin are later scraped with a sterile No. 15 Scalpel blade, being careful not to let the blade touch the eyelid or conjunctiva. Vigorous scraping is not performed in descemetocele cases.
- Smear preparation involves spreading the scraped corneal ulcer material onto glass slides. The smear is next allowed to dry in the air before being heat-fixed by being passed gently over a flame a couple of times. Gram's staining is done on the heat-fixed slides.
• Gram’s staining:
- Spray methyl violet over the smear and leave for 30 to 60 seconds.
- Pour the stain away and use Gram's iodine to cleanse. Put Gram's Iodine on top and wait for 30 - 60 seconds.
- Rinse the iodine with the decolorizer (acetone or alcohol) until the colour stops leaking from the smear. It takes less than ten seconds to complete this.
- After washing with water, counter-stain for 30 to 60 seconds with safranin, neutral red, or diluted carbol fuchsin.
- Rinse again with water, dry in the air, and examine while submerged in oil.
Gram negative bacteria are pink, while gram positive bacteria are violet. Gram’s stain provides the clearest illustration of yeast-like fungi, such as Candida. They resemble developing Gram-positive cells [20].
- 10% KOH Mount: One or two drops of 10% KOH solution are applied over the smear, a cover glass is placed carefully on top to prevent air bubbles, and the sample is then viewed under a microscope.
- Sabouraud’s agar: Corneal scrapings from the ulcer were injected into two slopes of Sabouraud's agar. One was kept at 25 degrees Celsius while the other kept at ambient temperature [13,21]. The growth is seen every day. The organisms were identified by colonial characteristics, microscopy, and biochemical changes after at least 48 hours [22]. The kind of mycelium, spore formation pigmentation, chlamydospore generation on corneal agar, etc. served to identify the organism [23]. The biochemical processes were then carried out to verify the species types. To develop the fungus, the cultures are repeated every 4 to 7 days [24]. Prior to certifying a case as an ulcer caused by a fungus, at least two cultures must be obtained [25] Table 1.
| Table 1: Incidence of corneal ulcers in our OPD. | ||
| Census | No. of cases | Percentage (%) |
| OPD patients | 800 | 100% |
| Corneal microbial keratitis | 90 | 11.25% |
| Keratomycosis | 8 | 8% |
Fungal corneal ulcers were discovered to be more common in the current investigation. It might be caused by the current widespread usage of stronger antibiotics and local steroids after eye injuries from agriculture.
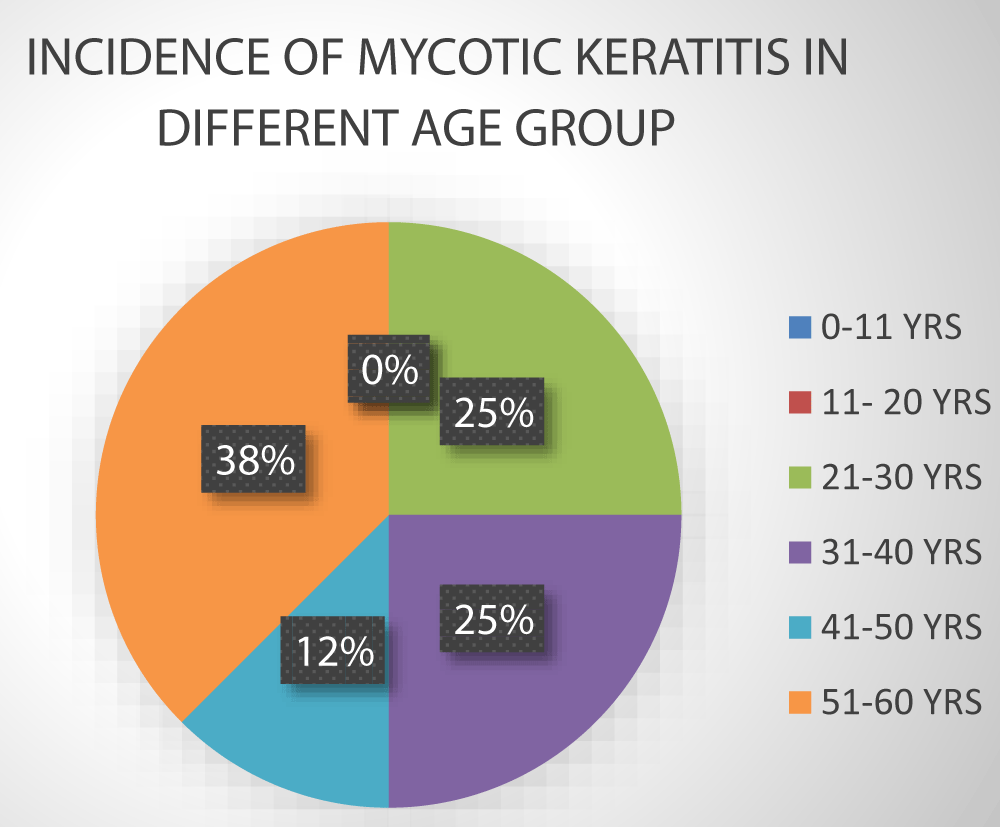
Incidence of age
The age incidence of keratomycosis in the current study shows (Table 2) that the age range of 51 to 60 years has the highest incidence (3), followed by 21 to 30 years (2), 41 to 50 years (1), 31 to 40 years (2), 11 to 20 years (0) and 0 to 10 years (0).
| Table 2: Age incidence of keratomycosis. | |||
| S.NO | Age group | No.of cases | Percentage (%) |
| 1 | 0-10 years | 0 | 0% |
| 2 | 11-20 years | 0 | 0% |
| 3 | 21-30 years | 2 | 25% |
| 4 | 31-40 years | 2 | 25% |
| 5 | 41-50 years | 1 | 12.5% |
| 6 | 51-60 years | 3 | 37.5% |
Due to the majority of agricultural workers working in the fields neglecting to seek medical attention when injured, cases are most prevalent in people between the ages of 50 and 60.
Sex incidence
In this study, there were 5 affected males (62.5%) and 3 affected females (37.5%). Males were more severely impacted than females. The ratio of men to women was 3:2 Table 3.
| Table 3: Sex incidence of keratomycosis | ||
| Sex | No .of Cases | Percentage (%) |
| Male | 5 | 62.5% |
| Female | 3 | 37.5% |
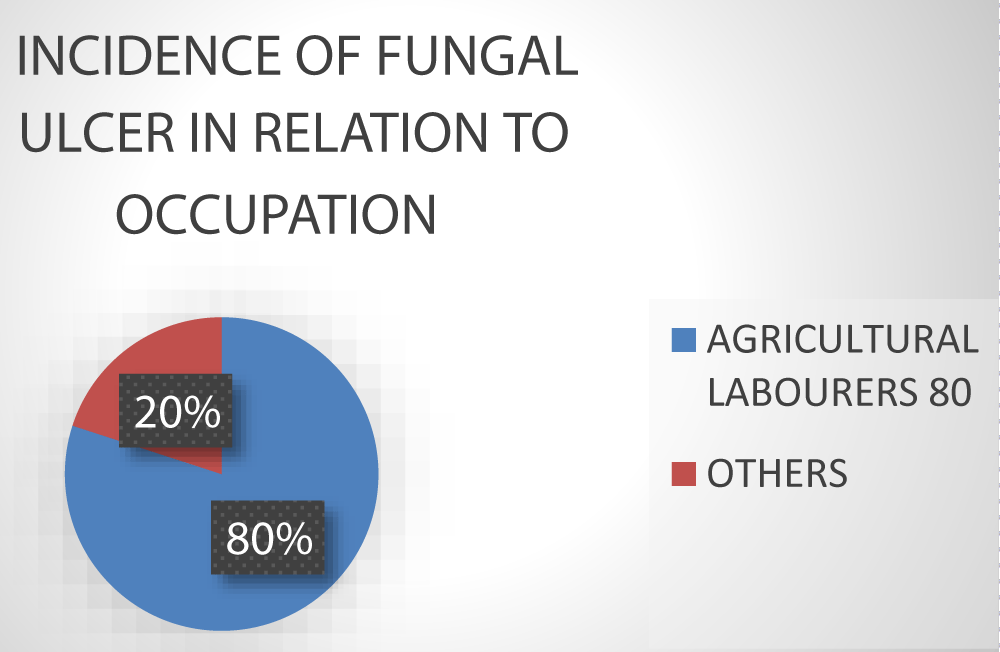
Incidence of fungal ulcer in relation to occupation
In the current study, agricultural labourers have the highest incidence of fungal ulcers [6], i.e. 80%, others (20%, or 2 cases) (Rickshaw drivers, students, and business people) Table 4.
| Table 4: Incidence of fungal ulcer in relation to occupation. | ||
| Occupation | No.of cases | Percentage (%) |
| Agricultural Labourers | 6 | 80% |
| Others | 2 | 20% |
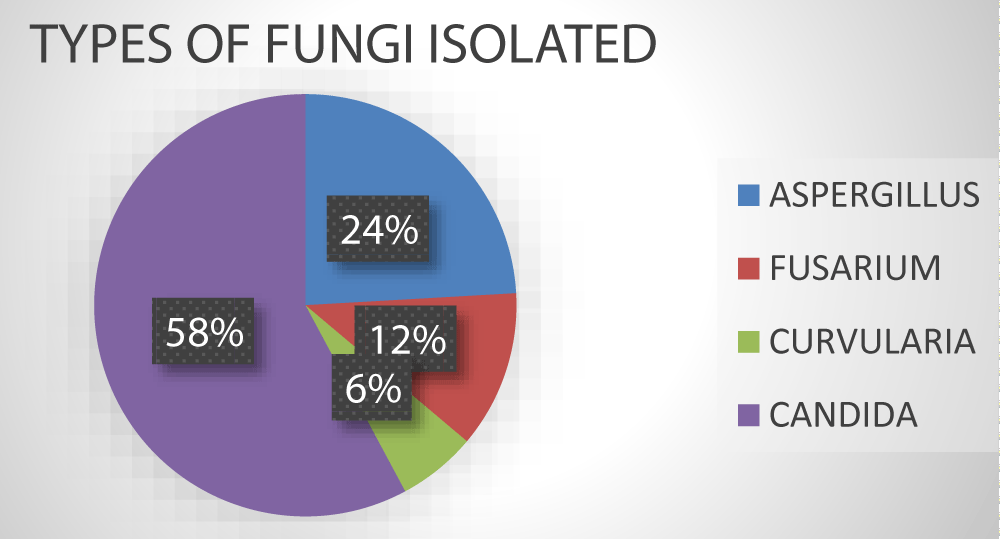
Incidence of various fungi along with species variation (Table 5).
| Table 5: Types of fungi isolated in the present series. | ||
| Fungi isolated | No of cases | Percentage (%) |
| Aspergillus | 4 | 50% |
| Fusarium | 2 | 25% |
| Curvularia | 1 | 12.5% |
| Candida | 1 | 12.5% |
Effect of antifungal agents: The current investigation revealed that Fluconazole is effective against Candida Albicans and Natamycin 5% eye drops are effective against Aspergillus species [26].
All of the straightforward fungal corneal ulcers, or those lacking hypopyon, responded well to natamycin eye drops [27] Table 6.
| Table 6: Effect of antifungal agents against various fungal species. | ||
| S.NO | Anti-Fungal agent | Targeted Species |
| 1 | 5% Natamycin | Aspergillus, Fusarium, Curvularia. |
| 2 | 0.3% Fluconazole | Candida |
Mycotic keratitis is a condition that affects a lot of people. This retrospective clinical study was conducted to determine the prevalence of corneal ulcers among various age groups, sexes, and occupations [9,10]. This study also addresses the impact of the antifungal medications Natamycin & Fluconazole.
8.8% of the corneal ulcers in our study were mycotic, out of the total. Today’s indiscriminate topical steroid use and increased antibiotic use as a result of agricultural eye injury during cultivation are to blame for the increased occurrence of fungal corneal ulcers [23]. Keratomycoses and systemic mycoses are becoming more common everywhere in the world. The crowded continents of Asia and Africa are seeing an increase in the occurrence of fungal keratitis. One of the main causes of vision loss and blindness, according to the World Health Organization, is corneal illness [28].
An estimated 1.5 to 2 million new cases of corneal blindness occur each year as a result of ocular trauma and corneal ulcers [12,13]. According to a study by Bibhudutta Rautaraya, et al. Mycotic keratitis is a major contributor to corneal blindness worldwide, including in India. The profile of fungal illnesses is known to be influenced by geographic location and climate. India’s tropical environment makes fungus-caused corneal ulcers frequent [29].
According to Badiee P, et al. economic and climatic factors are associated to the epidemiological variance and vast geographic distributions. Mycotic keratitis involving the cornea can cause significant visual damage or perhaps blindness and is challenging to treat [30]. Although it is widespread throughout the planet, the tropics and subtropics are where it is most prevalent [31].
The main risk factor is trauma [32], which is then followed by ocular and systemic abnormalities, previous corticosteroid usage, and extended use of antibiotic eye drops. The condition was more prevalent in people between the ages of 51 and 60. The fact that most patients at our hospital come from rural backgrounds may be the cause.
Here, there were 3 (37.5%) girls and 5 (62.5%) males who were afflicted. More men than women were impacted. The gender ratio is 3:2. Males have a higher frequency since they are exposed to more outdoor activities and visit hospitals more frequently.
Some of the fungi enter the corneal stroma [33]. In conditions like herpes keratitis, even minor damage to any vegetative material can quickly lead to a subsequent fungal infection [34]. Additionally, diabetes mellitus is the primary risk factor, and corticosteroid users are more susceptible to a fungal infection [35]. In this group of patients, it was thought that a special risk factor for a fungal infection of the cornea was trauma from plant material. Fungi that have been contaminated with them can enter the anterior chamber or the posterior section and damage the tissue using specialised mechanisms including proteolytic enzymes and mycotoxins.
The prognosis of this illness will be improved by a thorough understanding of the agent and host variables involved in these infections. The most typical fungus found was Aspergillus flavus, followed by Fusarium solani. Human fungal corneal ulcers are frequently brought on by filamentous fungus [36].
The aetiological agents of fungal keratitis have been determined to be more than 105 species of fungi, grouped into 56 genera [37]. A deep and serious corneal ulcer can be brought on by fungal keratitis. Aspergillus spp., Fusarium spp., Candida spp., Rhizopus, Mucor, and other fungus are responsible for its development [38].
Empirical treatment with broad-spectrum antibiotics may not always produce the best results [39]. Treatment based on accurate bacterial identification by culture and sensitivity assessment may. In order to customise therapy for patients who fail empirical therapy, culture results are also crucial [40]. The medicine of preference for topical therapy is natamycin suspension (5 mg/mL).
A topical antifungal drug along with systemic antifungal medications [41] were used in the treatment of patients with immunological disorders and those who have severe infections. Topical medications should be used hourly at first, then modified according on the outcome [30]. Typically, four weeks of intensive therapy are required [31].
When treating fungal keratitis, natamycin was a better option, particularly in the early stages of Fusarium infections [42]. The most effective medication for fungal keratitis involves topical antifungal drops like Natamycin and topical amphotericin B [43]. The gold standard for the treatment of fungal keratitis has not yet been identified [15,44]. Therapeutic penetrating keratoplasty is required for acute corneal perforation and vision recovery. Three kinds of antifungal medications are used to treat fungal keratitis: polyenes, triazoles and echinocandins. Prior to natamycin development, a polyene, Amphotericin B 0.15% was used in dilution with sterile water [17]. The most crucial agent in the treatment of fungal keratitis is thought to be the tetraene polyene 5% natamycin. Due to the easy and ready availability of natamycin, it has been chosen in this study. It works by forming a bond with ergosterol, a crucial element of the fungal cell wall and inhibiting microbial development [45]. Other antifungals including azoles like fluconazole are not active against Fusarium [46-86].
Out of 800 patients who attended Saveetha medical college and hospitals between January 2021 and June 2021, 90 incidences of corneal ulcers were found for this study. Eight of the 90 patients with corneal ulcers who were admitted to the patient department for treatment had positive fungal cultures in Sabouraud’s media. The age range of 50 to 60 years had a high prevalence of illness.
There were 90 total cases of corneal ulcers. There were 8 (8.8%) incidences of fungal ulcers out of those. More men than women were impacted. Workers in agriculture are more impacted than others.
The main cause of a fungus-induced corneal ulcer is trauma. More filamentous fungus than yeast are found. All filamentous fungus were dominated by Aspergillus species. Ulcers with a mix of bacteria and fungi were also found. People with impaired immune systems and diabetes were most affected.
Natamycin was the better option for the treatment of fungal keratitis. Filamentous fungi (Aspergillus species, fusarium, and curvularia) responded effectively to Natamycin 5% eyedrops. Cases that received good responses revealed corneal opacity. The medications utilised in the current RCTs differed from one another, and the small sample size made it difficult to determine which agent was more successful for treating fungal keratitis.
- Yanoff, Duker's Third Edition of Ophthalmology. 203.
- Kanski JJ. Clinical ophthalmology: a methodical method 168. 1993, and 1994,
- Balakrishnan E. MYCOTIC KERATITIS CAUSED BY ASPERGILLUS FUMIGATUS. Br J Ophthalmol. 1961 Dec;45(12):828-30. doi: 10.1136/bjo.45.12.828. PMID: 18170746; PMCID: PMC510167.
- Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79(3):214-21. Epub 2003 Jul 7. PMID: 11285665; PMCID: PMC2566379.
- Sharma S, Srinivasan M, George C. The current status of Fusarium species in mycotic keratitis in South India. J Med Microbiol. 1993; 11: 140–147.
- Upadhyay MP, Karmacharya PC, Koirala S, Tuladhar NR, Bryan LE, Smolin G, Whitcher JP. Epidemiologic characteristics, predisposing factors, and etiologic diagnosis of corneal ulceration in Nepal. Am J Ophthalmol. 1991 Jan 15;111(1):92-9. doi: 10.1016/s0002-9394(14)76903-x. PMID: 1985498.
- Dunlop AA, Wright ED, Howlader SA. Suppurative corneal ulceration in Bangladesh: a study of 142 cases looking at the clinical and epidemiological characteristics of bacterial and fungal keratitis. Aust N Z J Ophthalmol. 1994; 22:105–110.
- Leck AK, Thomas PA, Hagan M, Kaliamurthy J, Ackuaku E, John M, Newman MJ, Codjoe FS, Opintan JA, Kalavathy CM, Essuman V, Jesudasan CA, Johnson GJ. Aetiology of suppurative corneal ulcers in Ghana and south India, and epidemiology of fungal keratitis. Br J Ophthalmol. 2002 Nov;86(11):1211-5. doi: 10.1136/bjo.86.11.1211. PMID: 12386069; PMCID: PMC1771352.
- Hagan M, Wright E, Newman M, Dolin P, Johnson G. Causes of suppurative keratitis in Ghana. Br J Ophthalmol. 1995 Nov;79(11):1024-8. doi: 10.1136/bjo.79.11.1024. PMID: 8534648; PMCID: PMC505322.
- Liesegang TJ, Forster RK. Spectrum of microbial keratitis in South Florida. Am J Ophthalmol. 1980 Jul;90(1):38-47. doi: 10.1016/s0002-9394(14)75075-5. PMID: 7395957.
- Xie L, Shi W. Dongx: Penetrating keratoplasty in the treatment of fungal keratitis. Chin J Ophthalmol. 1994; 35:386-387.
- Coster DJ, Wilhelmus K, Peacock J. Suppurative keratitis in London Fourth European Society of Ophthalmology Congress, London: 1981, 395–398. International Congress and Symposium Series No. 40 of the Royal Society of Medicine.
- Asbell P, Stenson S. Ulcerative keratitis: study of 30 years of laboratory experience. Arch Ophthalmol. 1982; 100:77–80.
- Shokohi T, Nowroozpoor-Dailami K, Moaddel-Haghighi T. Fungal keratitis in patients with corneal ulcer in Sari, Northern Iran. Arch Iran Med. 2006 Jul;9(3):222-7. PMID: 16859055.
- FlorCruz NV, Peczon IV, Evans JR. Medical interventions for fungal keratitis. Cochrane Database Syst Rev. 2012 Feb 15;(2):CD004241. doi: 10.1002/14651858.CD004241.pub3. Update in: Cochrane Database Syst Rev. 2015;(4):CD004241. PMID: 22336802.
- Banerjee AR, Agarwal PK, Roy P, Das A, Banerjee A, Maity PK. Effectiveness of itraconazole as a broad-spectrum antifungal in mycotic corneal ulcers, both topically and internally. A first analysis. Indian Journal of Ophthalmology. 1999; 49(3):173-176.
- Mohan M, Sachdev MS, Gupta SK, Kalra VK, Vajpayee RB. The use of silver sulphadiazine for mycotic keratitis therapy. Indian J Med Res; 1987;85(1):572-575.
- Panda A, Sharma N, Das G, Kumar N, Satpathy G. Mycotic keratitis in children: epidemiologic and microbiologic evaluation. Cornea. 1997 May;16(3):295-9. PMID: 9143801.
- Gopinathan U, Sharma S, Garg P, Rao GN. Review of microbial keratitis epidemiological characteristics, microbiological diagnosis, and treatment outcome: over ten years of experience. Indian Journal of Ophthalmology. 2009; 57: 273–279.
- Bharathi MJ, Palaniappan R, Vasu S, Meenakshi R. aspects of the disease's epidemiology and a laboratory diagnosis of fungus keratitis. 3 years of research. Indian Journal of Ophthalmology, 2003; 51(4):315-321.
- Chander J, Chakrabarti A, Sharma A, Saini JS. Panigarhi Calcofluor staining evaluation for the identification of a fungal corneal ulcer. Mycoses; 1993;36(7-8):243-5.
- Poole TR, Hunter DL, Maliwa EM, Ramsay AR. Aetiology of microbial keratitis in northern Tanzania. Br J Ophthalmol. 2002 Aug;86(8):941-2. doi: 10.1136/bjo.86.8.941. PMID: 12140229; PMCID: PMC1771226.
- Srinivasan R, Kanungo R, Goyal JL. Spectrum of oculomycosis in South India. Acta Ophthalmol (Copenh). 1991 Dec;69(6):744-9. doi: 10.1111/j.1755-3768.1991.tb02053.x. PMID: 1789089.
- Sachdev MS, Mohan R. Indian Journal of Ophth. 1988; 495–498.
- Ormerod LD, Hertzmark E, Gomez DS. Multivariate investigation of the epidemiology of microbial keratitis in southern California. Ophthalmology. 1987; 4:1322-1333.
- Alfonso EC, Cantu-Dibildox J, Munir WM, Miller D, O'Brien TP, Karp CL. Fusarium keratitis outbreak linked to contact lens use. Fungal keratitis. Arch Ophthalmol. 2006; 124(7):941-947.
- Alexandrakis G, Jalali S, Gloor P. Polymerase chain reaction-based diagnosis of Fusarium keratitis in an animal model. Br J Ophthalmol. 1998; 82: 306–311.
- Ibrahim MM, Vanini R, Ibrahim FM, Fioriti LS, Furlan EM, Provinzano LM, De Castro RS, Sousa SJ, Rocha EM. Epidemiologic aspects and clinical outcome of fungal keratitis in southeastern Brazil. Eur J Ophthalmol. 2009 May-Jun;19(3):355-61. doi: 10.1177/112067210901900305. PMID: 19396778.
- Nath R, Baruah S, Saikia L, Devi B, Borthakur AK, Mahanta J. Mycotic corneal ulcers in upper Assam. Indian J Ophthalmol. 2011 Sep-Oct;59(5):367-71. doi: 10.4103/0301-4738.83613. PMID: 21836342; PMCID: PMC3159318.
- Lai J, Pandya V, McDonald R, Sutton G. Voriconazole and amphotericin B are administered intracamerally to treat the concomitant fungal iris nodule and fusarium keratitis. Clin Exp Opthalmol; 2014; 97(2):181–183;
- Florcruz NV, Peczon I Jr. Medical interventions for fungal keratitis. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD004241. doi: 10.1002/14651858.CD004241.pub2. PMID: 18254043.
- Mellado F, Rojas T, Cumsille C. Queratitis fúngica: revisión actual sobre diagnóstico y tratamiento [Fungal keratitis: review of diagnosis and treatment]. Arq Bras Oftalmol. 2013 Jan-Feb;76(1):52-6. Spanish. doi: 10.1590/s0004-27492013000100016. PMID: 23812531.
- Basak SK, Basak S, Mohantha A, Diagnoses of suppurative keratitis in Gangetic West Bengal, East India, based on epidemiology and microbiology. Indian Journal of Ophthalmology. 2005; 53(1):17–22.
- Bhartiya P, Daniell M, Constantinou M, Islam FMA, Taylor HR. Melbourne keratitis caused by fungi. Clin Experiment Ophthalmol. 2007; 35(2): 124–130.
- Gopinathan U, Garg P, Fernandes M. A 10-year assessment at a referral eye care centre in South India of the epidemiological characteristics and laboratory findings of fungal keratitis. Cornea. 2002; 21: 555-559.
- Rahman MR, Minassian DC, Howlader SA, Husain R., and Johnson GJ. A randomised trial using 2.5% natamycin and 0.2% chlorhexidine gluconate was conducted in Bangladesh for fungal keratitis. Br J Ophthalmol. 1998; 82(8):919–925.
- Tuli SS, Yoo SH. Curvularia keratitis after laser in situ keratomileusis from a feline source. J Cataract Refract Surg. 2003 May;29(5):1019-21. doi: 10.1016/s0886-3350(02)01608-5. PMID: 12781293.
- Garg P, Gopinathan U, Choudhary K, Rao GN. Keratomycosis: clinical and microbiologic experience with dematiaceous fungi. Ophthalmology. 2000 Mar;107(3):574-80. doi: 10.1016/s0161-6420(99)00079-2. PMID: 10711898.
- Mohan M, Sachdev MS, Gupta SK, Kalra VK. A novel treatment for ocular keratomycosis is topical silver sulphadiazine. Br J Ophthalmol; 1988; 72(3):192-195 77.
- El-Mofty HM, Khalil IA, Abdelhakim MA, El-Miligi MF, El-Nabarawi MA. An experimental investigation on a novel combination therapy for the treatment of fungal keratitis. J Ophthalmol; 2014(3):173298.
- Alfonso EC, Cantu-Dibildox J, Munir WM, Miller D, O'Brien TP, Karp CL, Yoo SH, Forster RK, Culbertson WW, Donaldson K, Rodila J, Lee Y. Insurgence of Fusarium keratitis associated with contact lens wear. Arch Ophthalmol. 2006 Jul;124(7):941-7. doi: 10.1001/archopht.124.7.ecs60039. Epub 2006 Jun 12. PMID: 16769827.
- Lalitha P, Vijaykumar R, Prajna NV, Fothergill AW. In vitro natamycin susceptibility of ocular isolates of Fusarium and Aspergillus species: comparison of commercially formulated natamycin eye drops to pharmaceutical-grade powder. J Clin Microbiol. 2008 Oct;46(10):3477-8. doi: 10.1128/JCM.00610-08. Epub 2008 Aug 13. PMID: 18701666; PMCID: PMC2566114.
- Vemuganti GK, Garg P, Gopinathan U, Naduvilath TJ, John RK, Buddi R, Rao GN. Evaluation of agent and host factors in progression of mycotic keratitis: A histologic and microbiologic study of 167 corneal buttons. Ophthalmology. 2002 Aug;109(8):1538-46. doi: 10.1016/s0161-6420(02)01088-6. PMID: 12153808.
- Arora R, Gupta D, Goyal J, Kaur R. Voriconazole versus natamycin as primary treatment in fungal corneal ulcers. Clin Exp Ophthalmol. 2011 Jul;39(5):434-40. doi: 10.1111/j.1442-9071.2010.02473.x. Epub 2011 Jun 28. PMID: 21105974.
- Rasool BK, Salmo HM. For the treatment of fungal keratitis, clotrimazolebeta-cyclodextrin eyedrops were created and clinically tested. AAPS Pharm Sci Tech; 2012; 13(3):883-889.
- Mahdy RA, Nada WM, Wageh MM, Kader MA, Saleh MM, Alswad MM. Evaluation of the efficacy and safety of a combined therapy using subconjunctival fluconazole and topical amphotericin B to treat fungal keratitis. Cutan Ocul Toxicol; 2010;29(3):193-197.
- Thomas PA. Mycotic keratitis—an underappreciated mycosis. J Med Vet Mycol. 1994; 32(4):235-256. 19.
- Thomas PA. Mycotic keratitis: an underappreciated mycosis. J Med Vet Mycol. 1994; 32: 235-254.
- Thomas PA, Kaliamurthy J, Geraldine P. Diagnoses, treatment options, and pathophysiology of mycotic keratitis are currently being considered.
- Gonzalez CA, Srinivasan M, Whitcher JP. Incidence of corneal ulceration in South India's Madhurai district. Ophthalmic epidemiology. 1996; 3: 159-166.
- Singh K, Chowdhary A. North India's fungal keratitis spectrum. Cornea; 2005; 24(1): 8-15.
- Tilak R, Singh A, Maurya OP, Chandra A, Tilak V, Gulati AK. An examination of mycotic keratitis in India over a five-year period. J Infect Dev Ctries; 2010; 4(3):171-174.
- Gopinathan U, Garg P, Fernandes M, Sharma S, Athmanathan S, Rao GN. A 10-year evaluation at a referral eye care center in south India of the epidemiological characteristics and laboratory findings of fungal keratitis. Cornea; 2002; 21555–21559.
- Badiee P, Alborzi A, Farhoudi F. A instance of Candida mediastinitis following dental extraction. J Infect Dev Ctries. 2011; 5(1):75-78.
- Reddy PS, Satyendran OM, Satapathy M, Kumar HV, and Reddy PR. Keratitis due to fungus. Indian Journal of Ophthalmology; 1972; 20(3):101-108.
- Wagoner RC, Tuli SS, Iyer SA. New developments and results of treatment for fungal keratitis. Eye Contact Lens. 2006; 32:267–271.
- Gower EW, Keay LJ, Oechsler RA, Iovieno A, Alfonso EC, Jones DB, Colby K, Tuli SS, Patel SR, Lee SM, Irvine J, Stulting RD, Mauger TF, Schein OD. Trends in fungal keratitis in the United States, 2001 to 2007. Ophthalmology. 2010 Dec;117(12):2263-7. doi: 10.1016/j.ophtha.2010.03.048. Epub 2010 Jun 29. PMID: 20591493.
- Srinivasan M, Gonzales CA, George C, Cevallos V, Mascarenhas JM, Asokan B, Wilkins J, Smolin G, Whitcher JP. Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India. Br J Ophthalmol. 1997 Nov;81(11):965-71. doi: 10.1136/bjo.81.11.965. PMID: 9505820; PMCID: PMC1722056.
- Tanure MA, Cohen EJ, Sudesh S, Rapuano CJ, Laibson PR. Spectrum of fungal keratitis at Wills Eye Hospital, Philadelphia, Pennsylvania. Cornea. 2000 May;19(3):307-12. doi: 10.1097/00003226-200005000-00010. PMID: 10832689.
- Cruz OA, Sabir SM, Capo H. Childhood microbial keratitis. Ophthalmology. 1993; 100:192–196.
- Hoflin-Lima AL, Roizenblatt R. Bilateral fungal keratitis caused by therapeutic contact lenses. CLAO J. 2002; 28:149-150.
- Thomas PA. The most recent thinking on ocular mycoses. Clin Microbiol Rev. 2003; 16:730-797.
- Periman LM, Harrison DA, Kim J. Fungal keratitis after photorefractive keratectomy: delayed diagnosis and treatment in a co-managed setting. J Refract Surg. 2003 May-Jun;19(3):364-6. doi: 10.3928/1081-597X-20030501-15. PMID: 12777034.
- Verma S, Tuft SJ. Fusarium solani keratitis following LASIK for myopia. Br J Ophthalmol. 2002 Oct;86(10):1190-1. doi: 10.1136/bjo.86.10.1190. PMID: 12234908; PMCID: PMC1771310.
- Jones DB, Barraquer JI, Binder PS, Buxton JN, Fine Jones DB, Laibson PR. Plan for the first care of suspected microbial keratitis. Symposium on Surgical and Medical Corneal Disorders. Transactions of the Ophthalmology Academy of New Orleans. Mosby: St. Louis, 1980; 86-119.
- Alfonso EC, Miller D, Rosa RH. South Florida's evolving fungal keratitis spectrum Ophthalmology. 1994; 101: 1005–1013.
- Venugopal PL, Venugopal TL, Gomathi A, Ramakrishna ES, Ilavarasi S. Mycotic keratitis in Madras. Indian J Pathol Microbiol. 1989 Jul;32(3):190-7. PMID: 2777350.
- Sharma SL. Keratomycosis in corneal sepsis. Indian J Ophthalmol. 1981 Dec;29(4):443-5. PMID: 7346474.
- Mohan M, Gupta SK, Kalra VK, Vajpayee RB, Sachdev MS. Silver sulphadiazine in the treatment of mycotic keratitis. Indian J Med Res. 1987 May;85:572-5. PMID: 3311988.
- Puttamen S. Junior All-Indian Ophth Society. 1969; 17: 171.
- KAUFMAN HE, WOOD RM. MYCOTIC KERATITIS. Am J Ophthalmol. 1965 Jun;59:993-1000. PMID: 14292735.
- Thomas PA. Fungal infections of the cornea. Eye (Lond). 2003 Nov;17(8):852-62. doi: 10.1038/sj.eye.6700557. PMID: 14631389.
- Chang CW, Ho CK, Chen ZC, Hwang YH, Chang CY, Liu ST, Chen MJ, Chen MY. Fungi genus and concentration in the air of onion fields and their opportunistic action related to mycotic keratitis. Arch Environ Health. 2002 Jul-Aug;57(4):349-54. doi: 10.1080/00039890209601420. PMID: 12530603.
- Thomas PA. Fungal infections of the cornea. Eye (Lond). 2003 Nov;17(8):852-62. doi: 10.1038/sj.eye.6700557. PMID: 14631389.
- Akter L, Salam MA, Hasan B, Begum N, Ahmed I. Etiological agents of suppurative corneal ulcers: investigation of 56 instances. J Med Microbiol Bangladesh. 2009; 3(2):33–36.
- Wang L, Sun S, Jing Y, Han L, Zhang H, Yue J. Central China has a kind of fungal keratitis. Clin Experiment Ophthalmol; 2009;37(8):763-771.
- Jurkunas U, Behlau I, Colby K. Fungal keratitis: changing pathogens and risk factors. Cornea. 2009 Jul;28(6):638-43. doi: 10.1097/ICO.0b013e318191695b. PMID: 19512908.
- Arora U, Gill PK, Chalotra S. Fungal Profile of Keratomycosis. Journal of Bombay Hospital 2009;51(3):325-327.
- 63.Tilak R, Singh A, Maurya OPS, Chandra A, Tilak V, and Gulati AK . An examination of mycotic keratitis in India over a five-year period. J Infect Dev Ctries; 2010; 4(8):171-174.
- Cohen EJ, Yildiz EH, Abdalla YF, Elsahn AF, Rapuano CJ, Hammersmith KM. From 1999 to 2008, a review of fungal keratitis was made. Cornea; 2010;29(12):1406–1411.
- Nagarathnamma T, Ambica R, Devi A. Keratomycosis epidemiological characteristics and laboratory diagnosis. Int J Biol Med Res; 2013;4(1):2879–2883.
- Day S, Lalitha P, Haug AW, Fothergill V, Cevallos R. Vijayakumar. Antibiotics' efficacy against Aspergillus and Fusarium. Br J Ophthalmol; 2009: 93(1):116-119.
- Wang, Chen, Huang all scored 73. observation of Natamyc's healing power in a fungal corneal ulcer. International Eye Science Guoji Yanke Zazhi; 2010; 10 (4):744-745.
- Mohan M, Gupta SK, Kalra VK, Vajpayee RB, Sachdev MS. A novel treatment for keratomycosis is silver sulphadiazine. Indian Journal of Ophthalmology; 1987; 35 (5- 6):83-87.
- Neoh CF, Kong DC, Stewart K, Chen SC, Daniell M. Caspofungin eye drops are useful clinically for keratitis caused by fungi. Int J Antimicrob Agents; 2014; 44 (2):96-104.
- Mimouni M, Tam G, Paitan Y, Kidron D, Segev F. Safety and efficacy of intrastromal injection of 5% natamycin in experimental fusarium keratitis. J Ocul Pharmacol Ther. 2014 Sep;30(7):543-7. doi: 10.1089/jop.2014.0004. Epub 2014 Jun 11. PMID: 24919100.