More Information
Submitted: September 15, 2023 | Approved: September 23, 2023 | Published: September 25, 2023
How to cite this article: Minckler D, Lin KY, Yang MC. Clinically Observable Ocular Manifestations of Axonal Transport. Int J Clin Exp Ophthalmol. 2023; 7: 006-007.
DOI: 10.29328/journal.ijceo.1001052
Copyright Licence: © 2023 Minckler D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Axonal transport; Chronic open-angle glaucoma; Intraocular pressure; Visual fields; Cup/disc ratio; Nerve fiber layer defect
Clinically Observable Ocular Manifestations of Axonal Transport
Don Minckler*, Ken Y Lin and Michael C Yang
Gavin Herbert Eye Institute, 850 Health Science Road, Irvine CA 92697-5375, USA
*Address for Correspondence: Don Minckler, Gavin Herbert Eye Institute, 850 Health Science Road, Irvine CA 92697-5375, USA, Email: [email protected]
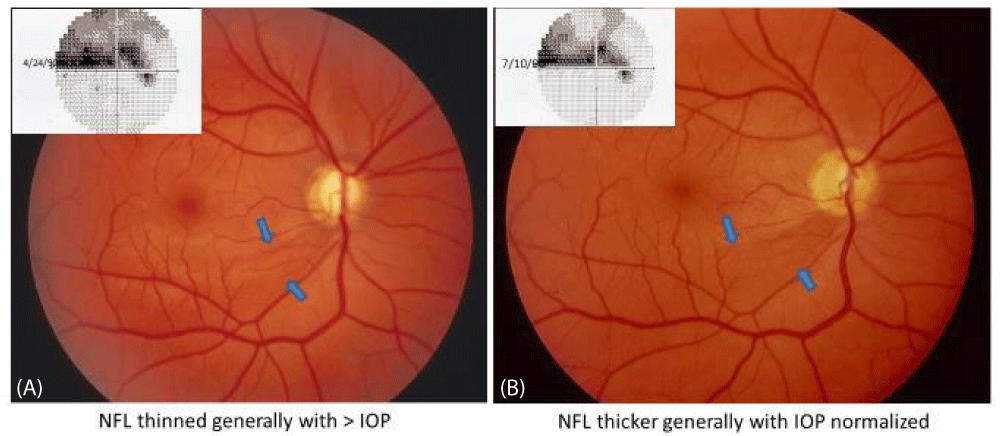
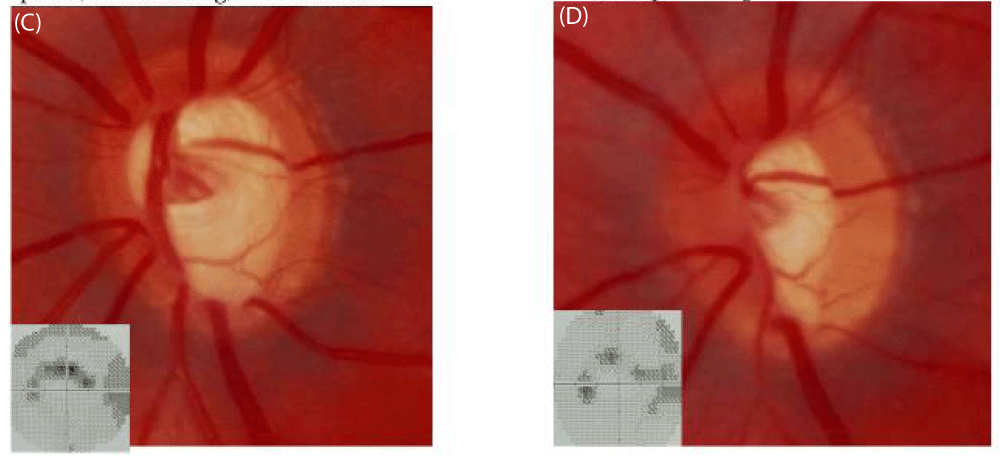
This report illustrates and provides a novel explanation for post-trabeculectomy improvements in the visual field, cup disc contours, and apparent deepening of an arcuate nerve fiber layer (NFL) defect after trabeculectomy for open-angle glaucoma. These changes are all plausible manifestations of recovered axonal transport and thickening retina, previously thinned by elevated intraocular pressure (IOP). Serial pre-and post-operative clinical fundus photos in case 1(A,B) demonstrate increased prominence of an inferior temporal arcuate nerve fiber layer defect, improved cup disc ratio, and visual field following eye pressure lowering by + 50% after trabeculectomy. Case 2 (C,D) also demonstrates obvious cup disc improvement in post-operative photos with associated improvement in visual field after trabeculectomy and lowering IOP by + 30%. We suggest that elevated IOP suppresses primarily orthograde axonal transport resulting in nerve fiber layer (NFL) thinning that can recover back to normal thickness when IOP is surgically lowered by the magnitude achieved in these two examples.
Case 1
Chronic open-angle glaucoma (COAG); elevated intraocular pressure (IOP); expanded cup/disc ratio; visual field defect (VFD).
Case 1: A. 29 yo M COAG IOP 30 mmHg; 7/14/89 Increased C/D ratio with sharpv temporal edge and prominent inferior temporal NFL defect outlined by arrows correlating with VFD. B. Same Eye 15 days post op Trabeculectomy 12/29/89 IOP 17 with accentuation of NFL defect, improved VF & decrease in C/D ratio, all thought due to recovery of prior suppression of axonal transport by high IOP.
Case 2
COAG and IOP 30 mmHg.
Case 2: C. 29 yo male IOP 30 mmHg OS COAG 7/10/90 > C/D ratio, pallor, undercutting, inferior notch. D. Same Eye 10 days after Trabeculectomy OS IOP 8-10 mmHg 7/20/90, persisting notch narrowed.
Numerous experimental studies in foveated primates with retinal and optic nerve anatomy identical to humans have demonstrated that elevated intraocular pressure blocks axonal transport in the lamina cribrosa (LC) [1]. The major causes of LC axonal transport impairment by elevated IOP include alterations in the trans-scleral pressure gradient by IOP, increased cerebral spinal fluid pressure (CSFP), and the relative rigidity of LC fibrous beams impinging on relatively flexible axonal membranes, i.e. a mechanical injury to axons triggering retinal ganglion cell death [2]. Disc recovery (reversible cupping) after treatment of glaucoma has been well documented, especially in children [3]. Vision and visual field recovery after glaucoma treatment have also been reported [4]. Clinical proof of our suggestion that the nerve fiber layer (or retinal thickness in general) is thinned by high IOP will depend on future ocular coherence tomography (sdOCT) studies of retinal thickness pre- and post-trabeculectomy ideally in relatively young adults [5]. Prior publications by David McLeod have hugely clarified the role of axonal transport in the pathogenesis of retinal cottonwool spots [6].
- Minckler DS, Bunt AH, Johanson GW. Orthograde and retrograde axoplasmic transport during acute ocular hypertension in the monkey. Invest Ophthalmol Vis Sci. 1977 May;16(5):426-41. PMID: 67096.
- Minckler DS, Brown DJ, Nalbandian A, Suh DW. Amyloid Precursor Protein in Abusive Head Trauma Suspects. Am J Ophthalmol. 2022 Aug;240:58-66. doi: 10.1016/j.ajo.2022.02.018. Epub 2022 Mar 2. PMID: 35247337.
- Quigley HA. Childhood glaucoma: results with trabeculotomy and study of reversible cupping. Ophthalmology. 1982 Mar;89(3):219-26. doi: 10.1016/s0161-6420(82)34803-4. PMID: 7088505.
- Katz LJ, Spaeth GL, Cantor LB, Poryzees EM, Steinmann WC. Reversible optic disk cupping and visual field improvement in adults with glaucoma. Am J Ophthalmol. 1989 May 15;107(5):485-92. doi: 10.1016/0002-9394(89)90492-3. PMID: 2712131.
- Yildirim E, Bilge AH, Ilker S. Improvement of visual field following trabeculectomy for open angle glaucoma. Eye (Lond). 1990;4 ( Pt 1):103-6. doi: 10.1038/eye.1990.12. PMID: 2323460.
- McLeod D. Why cotton wool spots should not be regarded as retinal nerve fibre layer infarcts. Br J Ophthalmol. 2005 Feb;89(2):229-37. doi: 10.1136/bjo.2004.058347. PMID: 15665358; PMCID: PMC1772507.