More Information
Submitted: May 06, 2024 | Approved: June 17, 2024 | Published: June 18, 2024
How to cite this article: Hassina S, Krichene MA, Hazil Z, Bekkar B, Hasnaoui I, et al. Exophthalmos Revealing a Spheno Temporo Orbital Meningioma. Int J Clin Exp Ophthalmol. 2024; 8: 001-003.
DOI: 10.29328/journal.ijceo.1001055
Copyright Licence: © 2024 Hassina S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Meningioma; Exophthalmos; Orbital; Spheno-temporal
Exophthalmos Revealing a Spheno Temporo Orbital Meningioma
Hassina S*, Krichene MA, Hazil Z, Bekkar B, Hasnaoui I, Robbana L, Bardi S, Akkanour Y, Serghini L and Abdallah EL
Ophthalmology B Specialty Hospital, Rabat, Morocco
*Address for Correspondence: Hassina S, Ophthalmology B Specialty Hospital, Rabat, Morocco, Email: [email protected]
Intracranial meningiomas are usually non-cancerous tumors that develop from arachnoid cells in the meningeal envelope. However, there are rare forms called intraosseous meningiomas, which present unique challenges for diagnosis and treatment. In this report, we describe a rare case of a giant sphenotemporal meningioma in a 72-year-old male with diabetes. The patient experienced progressive exophthalmos and visual impairment over a period of five months. Radiological imaging confirmed the diagnosis, showing extensive infiltration into the infra-temporal region. Histopathological examination confirmed a plaque-type meningothelial meningioma. The patient underwent surgical management, which involved maxillofacial surgery. Intraosseous meningiomas are rare but are increasingly being recognized, accounting for about two percent of all meningiomas. The spheno-orbital region is a common site for these tumors. Histologically, there are various subtypes, with meningothelial meningioma being the most common. The differential diagnosis includes Paget’s disease and osteomas. The optimal treatment approach involves extensive surgical resection, followed by adjuvant radiotherapy for any remaining or symptomatic tumors. The prognosis depends on the extent of resection and tumor progression, underscoring the importance of regular monitoring. Early intervention is crucial to preserve visual function and achieve favorable outcomes.
Extra-parenchymal tumors arising from the arachnoid cells of the meningeal envelope are known as intracranial meningiomas and generally have benign histology. A rare type of ectopic meningioma, intraosseous meningioma, accounts for less than 1% of all meningiomas [1]. Exophthalmos in a 72-year-old male patient revealed a rare case of giant sphenotemporal meningioma.
This is a 72-year-old diabetic patient on well-balanced oral antidiabetics who has been presenting with exophthalmos for 5 months with visual blur.
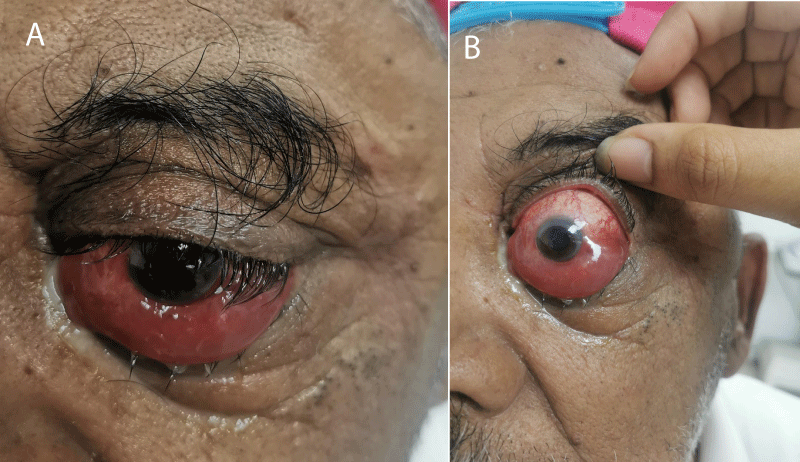
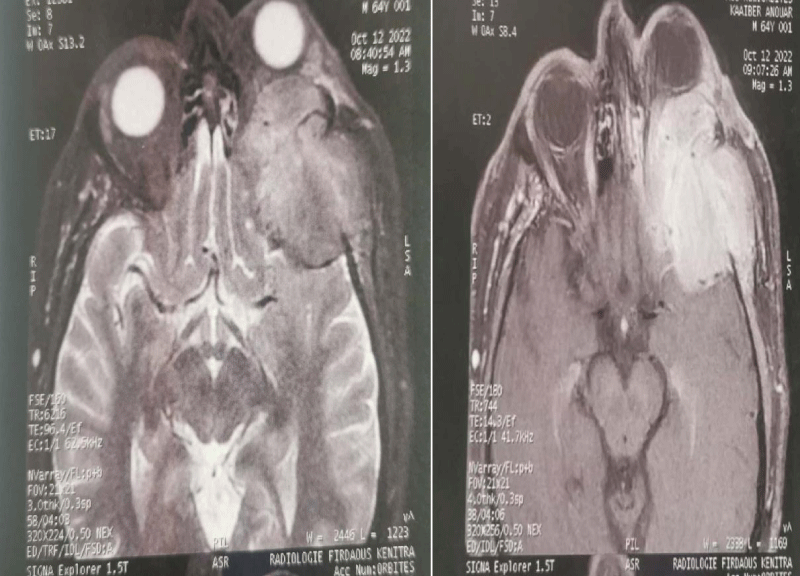
Ophthalmological examination finds right eye visual acuity at 3/10, normal segment anterior annexes, and a normal fundus. Left eye visual acuity is at 1/10 with non-pulsatile axial exophthalmos grade 3, inferior conjunctival chemosis (Figure 1A,B) and normal fundus. Clinical presentation required MRI revelation of spheno-temporo-orbital meningioma responsible for grade 3 exophthalmos and infra-temporal foundation invasion (Figure 2). Bone biopsy revealed, after an immunohistochemical study, a plaque-type meningothelial meningioma. The patient was referred to maxillo-facial surgery for management.
Figure 1: A,B: Exophtalmia grade 3 inferior conjunctival chemosis.
Figure 2: MRI revelation of spheno-temporo-orbital meningioma responsible for grade 3 exophthalmos and infra-temporal foundation invasion.
The number of published cases of meningiomas of primary extracranial origin has increased, approaching two percent of all meningiomas [2]. Fourteen percent are intraosseous tumors, identified as osteoblastic lesions or mixed forms with osteolytic components [1]. Classical osteolytic varieties are very rare, and the cases described correspond mainly to tumors of the skull. Ectopic meningiomas have been identified in the subcutaneous tissue of the skin, orbit, paranasal sinuses, salivary glands, etc. 2.c. This type of meningioma is called primary extradural meningioma, they are extremely rare.
The spheno-orbital and frontoparietal regions are the most common locations for intraosseous meningiomas. There are various hypotheses as to the origin of these cephalic intraosseous meningiomas. One hypothesis is that they develop from ectopic meningocytes or arachnoid capillaries trapped in the cranial sutures during embryonic development [3]. The second hypothesis is that meningothelial cells are also trapped in the sutures or in cranial fractures secondary to trauma [4].
Spheno-orbital meningiomas (soms) are extremely rare tumours characterized by pathological hyperostosis of the sphenoidal crest. The tumor’s bony invasion and proximity to and invasion of critical structures of the orbit, optic canal, superior orbital fissure (sof), and cavernous sinus result in a classic presentation of proptosis, decreased vision, abnormal ocular motility, ptosis, and headache. Exophthalmos is the most common clinical presentation and is generally slow-onset, non-pulsatile, irreducible, and painless. Epileptic seizures may appear later in the course of the disease [5].
Histologically, several subtypes can be distinguished: meningothelial meningioma (62.1%), transitional meningioma (18.2%), fibroblastic meningioma (6.1%), psammomatous meningioma (6.1%) and malignant meningioma (7.6%). In our case, the histological type was meningothelial [6].
The differential diagnosis is Paget’s disease, fibrous dysplasia, osteoma, osteoblastic metastases, or plaque meningioma [7].
Primary intraosseous meningiomas are benign lesions for which extensive surgical resection followed by cranial reconstruction is recommended. If this is not possible due to the proximity of vital structures, e.g. in the periorbital region, radiological follow-up of the residual tumour is recommended [8]. In cases of visual impairment, decompression of the optic canal is also strongly recommended [5]. Sof meningiomas with extension to the orbit are currently removed by several transcranial approaches, including supraorbital-perioral, frontotemporal-orbito-zygomatic, fronto-orbital-malar, and perioral [9].
Depending on the extent of resection of the orbital wall and roof, most authors who have performed these craniotomy variants recommend firm reconstruction of the orbital walls to avoid pulsatile enophthalmos and diplopia, we consider that reconstruction of the hyperostotic lateral orbital wall and temporal bone is not necessary in almost all cases operated on by lateral orbital mini-approach [10,11].
Fronto-temporo-sphenoidal craniectomy with resection of all invaded tissues, i.e. dura mater, muscle, and intraorbital tissues, with dural and parietal reconstruction, is the treatment of choice [12].
Adjuvant radiotherapy is recommended for patients with symptomatic and/or enlarging residual lesions [13].
The cure is inversely proportional to the degree of tumour extension. The slow rate of progression facilitates monitoring of tumour remnants and/or detection of recurrence by annual MRI check-ups. When visual function is affected, preoperative visual acuity and duration of progression are prognostic factors for postoperative functional recovery [14].
The management of primary intraosseous meningiomas, particularly spheno-orbital meningiomas, requires a multidisciplinary approach involving extensive surgical resection, careful monitoring, and, in some cases, adjuvant radiotherapy. The rarity of these tumors and their complex anatomical relationships necessitate individualized treatment plans to optimize outcomes and preserve function.
- Alcalá Cerra G, Moscote Salazar LR, Lozano Tangua CF, Sabogal Barrios R, García Quintana G. Primary osteolytic intra diploic meningioma: Case report. Rev Chil Neurosurgery [Internet]. 2010 [cited 2019 Dec 15]; 34(10).
- Ammirati M, Mirzai S, Samii M. Primary intraosseous meningiomas of the skull base. Acta Neurochir (Wien). 1990;107(1-2):56-60. doi: 10.1007/BF01402613. PMID: 2096610.
- Daffner RH, Yakulis R, Maroon JC. Intraosseous meningioma. Skeletal Radiol. 1998 Feb;27(2):108-11. doi: 10.1007/s002560050347. PMID: 9526778.
- Ichimura S, Hara K, Shimokawa R, Kagami H, Inaba M. A case of intraosseous microcystic meningioma without a mass lesion. Neurol Med Chir (Tokyo). 2013;53(10):699-702. doi: 10.2176/nmc.cr2012-0124. Epub 2013 Sep 24. PMID: 24064568; PMCID: PMC4508748.
- Nozaki K, Kikuta K, Takagi Y, Mineharu Y, Takahashi JA, Hashimoto N. Effect of early optic canal unroofing on the outcome of visual functions in surgery for meningiomas of the tuberculum sellae and planum sphenoidale. Neurosurgery. 2008 Apr;62(4):839-44; discussion 844-6. doi: 10.1227/01.neu.0000318169.75095.cb. PMID: 18496190.
- De Jesús O, Toledo MM. Surgical management of meningioma en plaque of the sphenoid ridge. Surg Neurol. 2001 May;55(5):265-9. doi: 10.1016/s0090-3019(01)00440-2. PMID: 11516463.
- Arregui R, Ovalle R, Castillo J. Extradural meningioma of middle ear: Reporting a case and literature review. Rev Otorrinolaringol Cir Cabeza Cuello. 2017; 77(4).
- Mariniello G, Maiuri F, de Divitiis E, Bonavolontà G, Tranfa F, Iuliano A, Strianese D. Lateral orbitotomy for removal of sphenoid wing meningiomas invading the orbit. Neurosurgery. 2010 Jun;66(6 Suppl Operative):287-92; discussion 292. doi: 10.1227/01.NEU.0000369924.87437.0B. PMID: 20489518.
- Al-Mefty O. Supraorbital-pterional approach to skull base lesions. Neurosurgery. 1987 Oct;21(4):474-7. doi: 10.1227/00006123-198710000-00006. PMID: 3683780.
- Ringel F, Cedzich C, Schramm J. Microsurgical technique and results of a series of 63 spheno-orbital meningiomas. Neurosurgery. 2007 Apr;60(4 Suppl 2):214-21; discussion 221-2. doi: 10.1227/01.NEU.0000255415.47937.1A. PMID: 17415156.
- Heufelder MJ, Sterker I, Trantakis C, Schneider JP, Meixensberger J, Hemprich A, Frerich B. Reconstructive and ophthalmologic outcomes following resection of spheno-orbital meningiomas. Ophthalmic Plast Reconstr Surg. 2009 May-Jun;25(3):223-6. doi: 10.1097/IOP.0b013e3181a1f345. PMID: 19454936.
- Van Tassel P, Lee YY, Ayala A, Carrasco CH, Klima T. Case report 680. Intraosseous meningioma of the sphenoid bone. Skeletal Radiol. 1991;20(5):383-6. doi: 10.1007/BF01267669. PMID: 1896882.
- Sandalcioglu IE, Gasser T, Mohr C, Stolke D, Wiedemayer H. Spheno-orbital meningiomas: interdisciplinary surgical approach, resectability and long-term results. J Craniomaxillofac Surg. 2005 Aug;33(4):260-6. doi: 10.1016/j.jcms.2005.01.013. PMID: 15978821.
- Brusati R, Biglioli F, Mortini P, Raffaini M, Goisis M. Reconstruction of the orbital walls in surgery of the skull base for benign neoplasms. Int J Oral Maxillofac Surg. 2000 Oct;29(5):325-30. PMID: 11071232.