More Information
Submitted: September 26, 2024 | Approved: October 08, 2024 | Published: October 09, 2024
How to cite this article: Elmajri KAK, Fathy A. Prevalence and Correlation between HbA1c Control and Duration of Diabetes with Blindness in the Eastern Part of Libya: Double Centers Study. Int J Clin Exp Ophthalmol. 2024; 8(2): 021-026. Available from: https://dx.doi.org/10.29328/journal.ijceo.1001058.
DOI: 10.29328/journal.ijceo.1001058
Copyright Licence: © 2024 Elmajri KAK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Prevalence and Correlation between HbA1c Control and Duration of Diabetes with Blindness in the Eastern Part of Libya: Double Centers Study
Khalid AK Elmajri1* and Abdolmejed Fathy2
1Faculty of Medicine, Always Teaching Hospital, Derna University, Libya
2Faculty of Medicine, Tobroke Hospital Center, Tobruk University, Libya
*Address for Correspondence: Khalid AK Elmajri, Assistant Professor, Faculty of Medicine, Derna University-Always Teaching Hospital, Libya, Email: [email protected]
A prospective cross-sectional study of diabetic patients registered at the Eye department of Tobruk Medical Center in Tobruk-Libya between (01.06.2023 to 29.02.2024). At the same time data was collected in the eye department in Alwahda Derna Teaching Hospital, Data was collected using the same administered questionnaire. Grading of DR was done by slit-lamp examination and Fundoscopy by an ophthalmologist. Descriptive analysis included percentage mean, median, and p - value by using SPSS 25. There were 185 diabetic patients, ages ranging between 30 and 90 years, with a mean of 58, the majority (97.6%) were of Libyan nationality. There were 86 males and 99 females. Patients with a duration of diabetes ranging between 11 and 15 years were at almost a five-fold risk of developing DR compared to those with a duration of < 10 years. Most of advanced complicated diabetic retinopathy cases had diabetes for more than fifteen years, and no advanced disease in the cases with a duration of less than 10 years.
The patients with poor controlled blood sugar and HbA1c > 9 throughout the disease were at almost five-folded risk of developing DR compared to those with moderate controlled diabetes cases were HbA1c between (7.5 - 9), patients with poor control of diabetes HbA1c> 9 was 25-folded risk of developing PRP than cases with good control HbA1c < 7.5. The majority of advanced diabetic retinopathy cases were correlated with non-controlled diabetes mellitus HbA1c > 9, where no advanced complication was recorded in well-controlled cases.
Diabetes mellitus is a chronic metabolic disease characterized by hyperglycemia/ hypoglycemia, damage to large blood vessels (macrovascular) like cardiovascular and cerebrovascular disease, and damage to the small blood vessels (microvascular) like nephropathy or retinopathy [1].
Diabetic retinopathy is one of the most common microvascular complications of diabetes mellitus. Diabetic retinopathy (DR) is a common cause of blindness among adults in the Western world [1,2].
Diabetic retinopathy in patients with type 1 (insulin-dependent DM) more than with type 2 (insulin-dependent DM), was found to be related to both the severity of hyperglycemia and the presence of other chronic diseases like hypertension [3]. Diabetic retinopathy is usually detected in late stages, because of the lack of awareness in our country about the risk of the disease as well as poor motivation for regular health care, diabetic patients in our community only come for consultation after the disease has become symptomatic. , good control of blood sugar in the blood, and effective diabetes management with diet and exercise can significantly decrease the progression of diabetic retinopathy [4]. Diabetic retinopathy is one of the leading causes of blindness worldwide. Because prolonged time and less control of blood sugar in blood damage the retinal blood vessels. In the early stages, diabetic retinopathy is usually asymptomatic, this results in a late diagnosis of DR, and patients do not come for consultation unless the irreversible progressive stage starts to progress with time to different stages if not managed early [5]. Several stages start from mild non-proliferative DR with small microaneurysms of retinal blood vessels to severe proliferative stages with the growth of new fragile retinal blood vessels which can lead to advanced blindness leading problems like vitreous hemorrhage, macular ischemia, and retinal detachment [6]. There are some treatment options which depending on the severity of the disease, starting with laser, injection of steroids or intra vitreous anti-VEGF, until pars plana vitrectomy in the advanced stages [7]. The objective of this study is to estimate the prevalence and identify the correlation between risk factors like age of patients, type of DM, duration, and control of diabetes mellitus patients with progression of DR attending the Eye Department at two centers Tobruk and Derna centers, eastern part of Libya.
The objective of this study is to estimate the prevalence and identify the correlation between risk factors like age of patients, type of DM, duration, and uncontrolled diabetes mellitus patients with blindness due to progression of DR attending the Eye Department at the two centers in eastern part of Libya.
A prospective cross-sectional study of diabetic patients registered at the Eye department in both centers at the same time between (01.06.2023 to 29.02.2024). Data was collected using the same-administered questionnaire. Grading of DR was done by slit-lamp examination and Fundoscopy by an ophthalmologist. Descriptive analysis included percentage mean, median, and p - value by using SPSS 25. Hba1c < 7.5% considered as controlled diabetic patients and > 7.5% poorly controlled diabetes mellitus patients. Diabetic retinopathy grading divided into non-proliferative diabetic retinopathy (mild, moderate, and severe), when complications start with new blood vessels in the retina is called proliferative diabetic retinopathy and when complications of PRP occur as neovascular glaucoma, vitreous hemorrhage, and tractional RD is advanced DRP. The diagnosis was done with Slit-lamp examination and lens Volk 78, 90 D and indirect ophthalmoscope and ultrasound. Detailed examination was performed by an experienced ophthalmologist. Visual impairment classification considered as WHO visual loss classification were good or normal vision considered > 0.8, mild visual impairment between (0.4 - 0.8), moderate visual impairment between (0.1 - 0.3), severe visual impairment between (> HM-0.05), subtotal blindness (HM or PL) and completely blindness no PL.
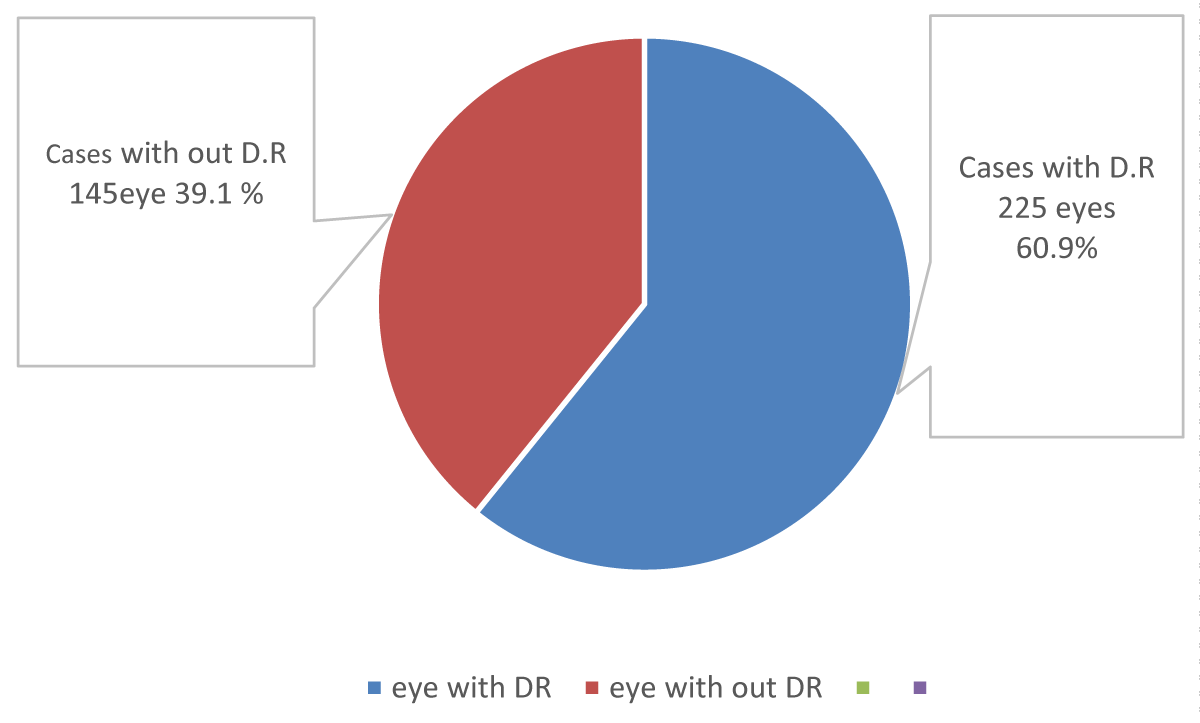
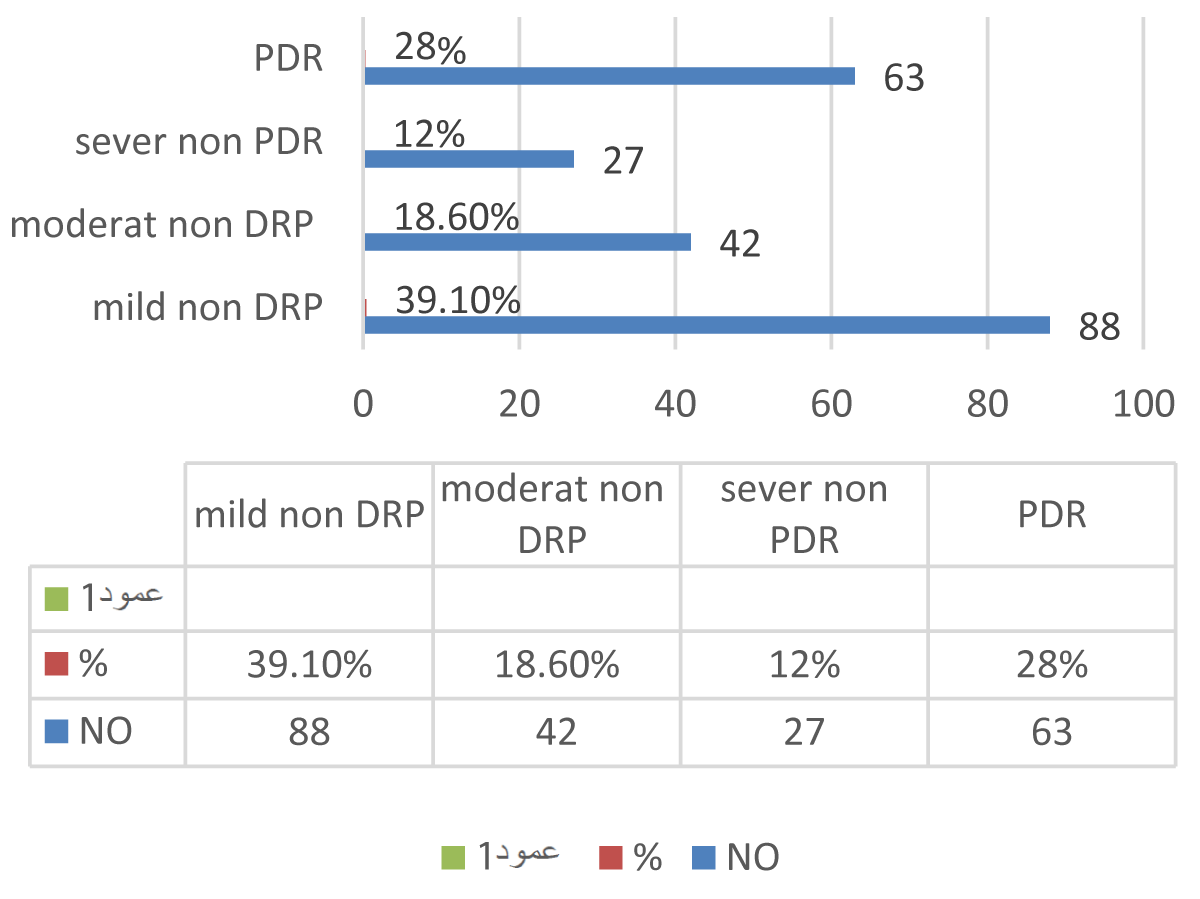
In this study; there were 370 cases of diabetic patients, ages ranging between 30 and 90 years, with a mean of 58 years, whereas the majority (97.6%) were Libyan nationality living in Tobruk and Derna city. The prevalence of diabetic retinopathy was 225 (60.8%) of the study cases and 145 cases escaped the condition. Mild non-DR was found in 88 cases (39.1% of all cases) s, whereas moderate non-proliferative retinopathy type was in 42 cases (18.6% of the cases), and severe non-proliferative diabetic retinopathy was noted among 27 cases (12%). Whereas proliferative type was considered in about 63 cases, 28 % of all cases studied (Figure 1).
Figure 1: Prevalence of diabetic retinopathy.
There were 31 out of 63 cases (49.2%) of proliferative diabetic retinopathy eyes, considered as advanced stages of PDR because these cases are complicated with severe complications of PDR as vitreous hemorrhage, neovascular glaucoma, and tractional retinal detachment;1 eyes presented with vitreous hemorrhage, 10 cases with retinal detachment and 6 with neovascular glaucoma (Figure 2).
Figure 2: Distribution of the types of Diabetic retinopathy according to stage.
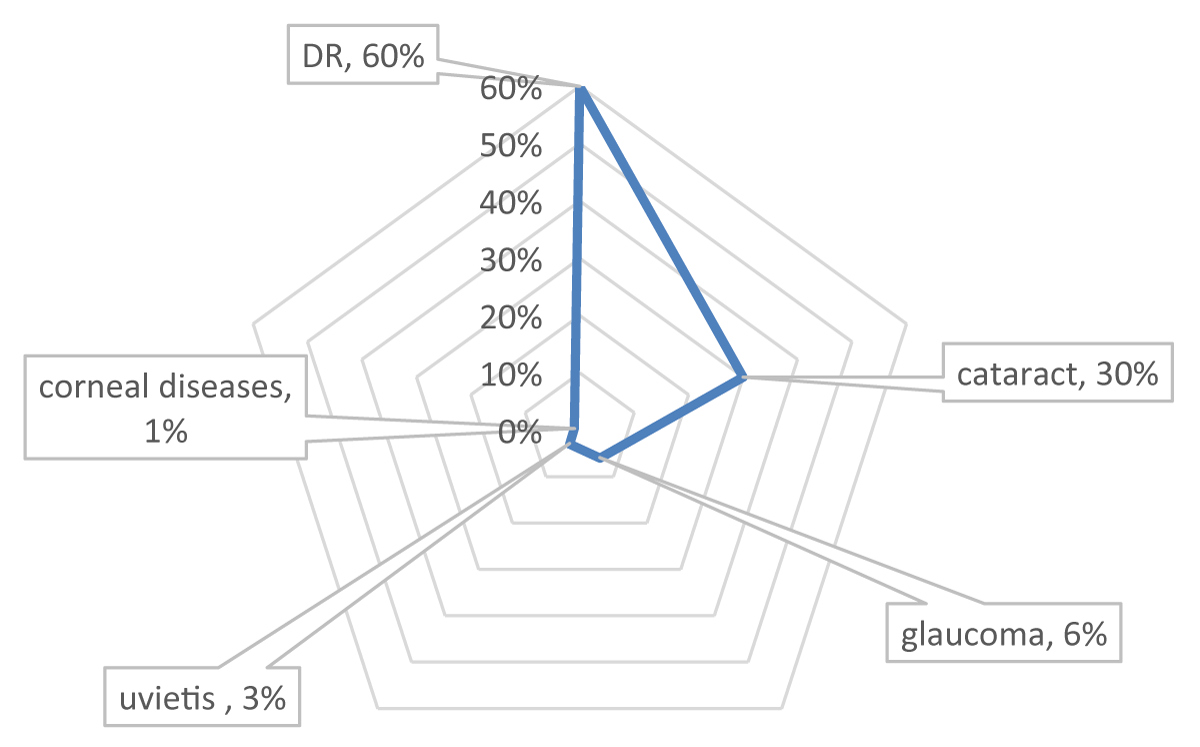
The most common visual impairment in diabetic patients was reported namely viz., diabetic retinopathy (DR) (60%), followed by cataracts (30%), glaucoma (6%), and uveitis (3%), and corneal diseases (1%). Systemic-associated diseases like systemic hypertension were observed in about (40%) and cardiac disease (13%) (Figure 3).
Figure 3: Visual impairment in diabetic patients.
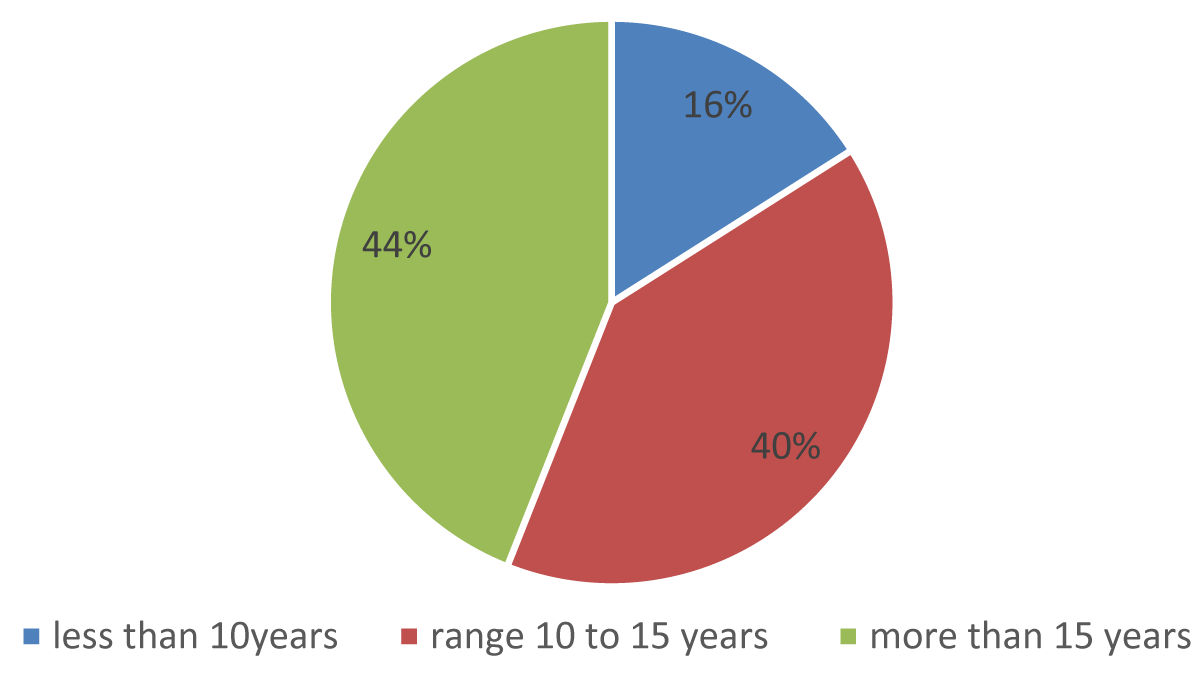
The duration of diabetes mellitus ranged between 5 and 40 years, there was (16%) duration of diabetes less than 10 years, whereas (44%) exceeded 15 years and (40%) ranged between 10 and 15 years. Type II Diabetes Mellitus (90.6%) which they treated with oral medication and diets, and type I-DM 9.4%.
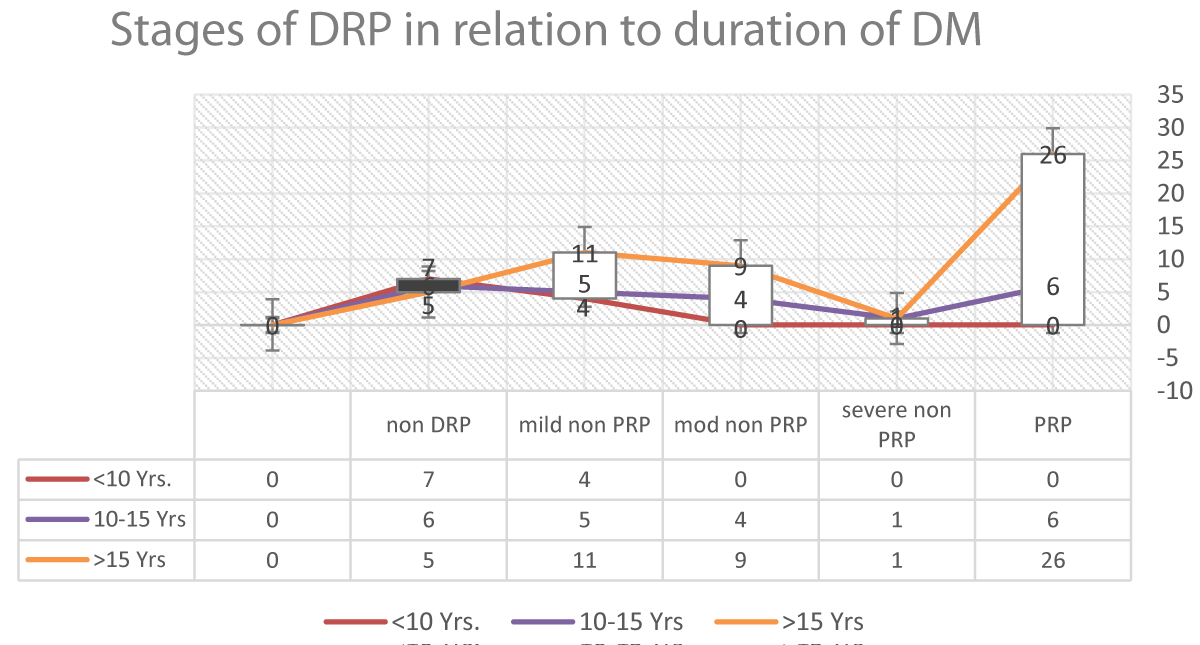
The results considered that cases with a duration of diabetes ranging between 11 and 15 years were at almost five-folded risk of developing DR compared to those with a duration less than 10years, where cases with a duration of diabetes more than 15 years two-folded risk of developing DR than cases with duration less than 15 years (Figure 4).
Figure 4: Duration of diabetes mellitus (in years).
In proliferative diabetic retinopathy (PR) most of the cases duration of diabetes is more than 15 Years, fivefold than the cases with duration of diabetes less than 15 Years.
Most advanced complicated diabetic retinopathy cases had diabetes of more than fifteen years, cases with a duration of diabetes between 10 - 15 years no more complication, and no advanced disease in the cases with duration of less than 10 years. The Figure 5 shows the progression of DRP concerning the duration of diabetes Miletus.
Figure 5: Progression of DRP concerning the duration of diabetes Miletus.
There were 142 cases (83.5%) with poor control of diabetes mellitus, where Hba1c > 7.5% throughout the diabetes and only 28 of the cases with controlled DM and Hba1c < 7.5% throughout the disease. Two cases out of eight of type I (IDDM) had controlled diabetes, where HbA1c does not exceed 7.5%.
Our study considered that cases with poorly controlled blood sugar and HbA1c > 9 throughout the disease were at almost five-folded risk of developing proliferative diabetic retinopathy compared to those with moderately controlled diabetes cases were HbA1c between (7.5 - 9), and patients with poor control of diabetes HbA1c > 9 were 25-folded risk of developing PR than cases with good control HbA1c < 7.5. The majority of not controlled cases were HbA1c > 7.5 throughout the disease and had some degree of diabetic retinopathy.
The majority of advanced diabetic retinopathy cases were correlated with non-controlled diabetes mellitus HbA1c > 9%, with only four cases with moderate control HbA1c between (7.5% - 9%). There were no advanced complications recorded in well-controlled cases.
Deterioration of vision as an indicator of function outcome of the eye was recorded in the majority of the cases. There were 64 tested eyes recorded as mild visual impairment, were visual acuity > 0.3 on the Snellen chart. Whereas moderate visual impairments were considered in 88 eyes (visual acuity between 0.1 - 03), severe visual impairment in 27 eyes, visual acuity between (0.05 - > HM), legal or subtotal blindness (vision HM or PL) resulted in 20 eyes, and total blindness (no PL) in 6 eyes of the study.
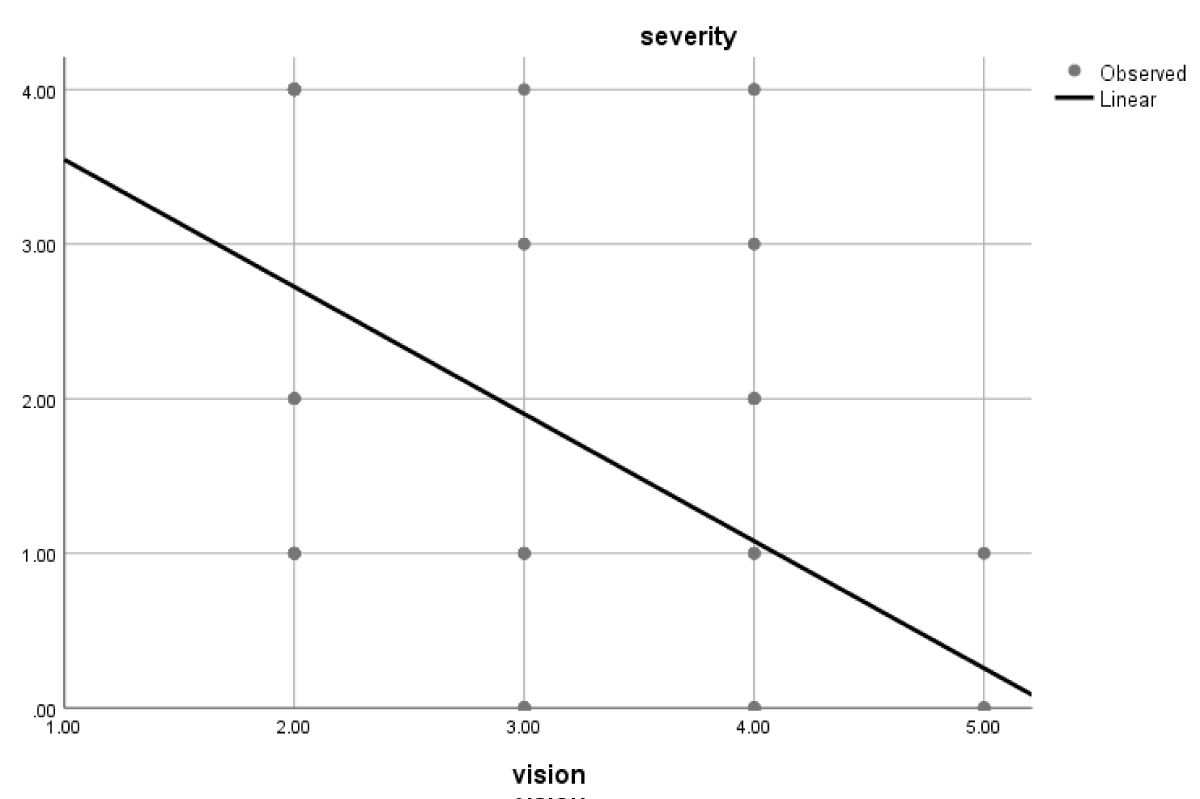
Deterioration of vision is statistically significantly related to poor stage of severe diabetic retinopathy. (p value 0.01) and significantly related to poor follow-up cases (p value 0.000) (Tables 1,2) (Figure 6).
Figure 6: The deterioration of vision with the severity of the disease.
| Table 1: Stages of diabetic retinopathy in compression to degree of diabetes control by patient's diet history and HBA1c control and blood sugar level. | |||||
| Degree of control of DM | Non DRP | Mild non PRP | Mod non PRP | Sever non PRP | PDRP |
| good controlled* | 18 | 10 | 4 | 2 | 8 |
| mod controlled* | 24 | 15 | 7 | 4 | 10 |
| non controlled* | 30 | 19 | 10 | 7 | 13 |
| *Good controlled HbA1c < 7.5, moderate controlled HbA1c (7.5 - 9), poor controlled HbA1c > 9. | |||||
| Table 2: Test Statisticsa | ||
| Vision - severity | Vision - follow-up | |
| Z | -3.317b | -3.925b |
| Asymp. Sig. (2-tailed) | 0.001 | 0 |
| aWilcoxon Signed Ranks Test. bBased on negative ranks. |
||
Deterioration of vision is related to the severity of the disease, look to Figure 4 Majority of advanced cases presented with severe visual impairment.
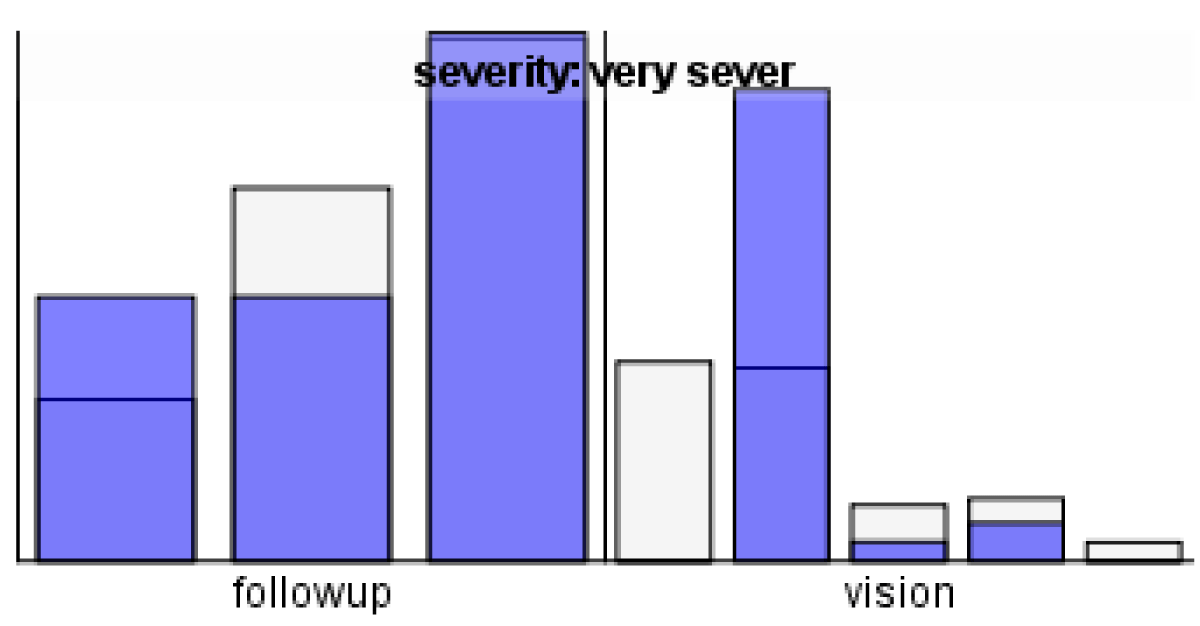
Patients with uncontrolled diabetes were at a significantly higher risk of developing advanced DR compared to those whose disease was well-controlled and had good follow-up (p < 0.001) (Figure 7).
Figure 7: The severity of diabetes Miletus and advanced DR.
Diabetic retinopathy is one of the diabetes mellitus complications that can lead to loss of vision if not early discovered and properly controlled. For this, we should know the DR problem and identify its associated risk factors, and routinely fundus examination, to detect the RP in the early stage, which is essential for the achievement of better management to improve the outcome [8].
Our study’s overall DR prevalence was 60.8%, which is almost higher than the projected global prevalence of 34.6% among people with diabetes that has been documented, but because most of the cases come to our department symptomatic and come to get a consultation, which can explain our higher prevalence [9] or could be related to the disaster that happened in that area (denial) eastern part of Libya at the time of this study which makes the follow-up or regularity of treatment not assessable or may be related to stress and type of lifestyle at that time
In general DR formation in diabetic patients was significantly associated with male patients, older age patients, long duration of disease, uncontrolled HbA1c, adherence to medications and unhealthy diet, irregular diabetes follow-up, irregular fundus examination, patients with history of HTN, dyslipidemia, chronic kidney disease, patients with diabetic complications (cataract, glaucoma, diabetic foot ulcer, renal insufficiency, Myocardial Infarction [MI], and heart failure), and patients with higher BMI and lower GFR. Patients’ nationality, marital status, place of residence, and family history of diabetes, were not significantly associated with the development of DR [10].
The most frequent risk factors for the detection of DR are a type of diabetes, disease duration, poor glycemic control (high HbA1c levels), and the presence of other systemic diseases like hypertension were associated with an increased probability of developing DR [11]. Other risk factors for developing DR include obesity, hyperlipidemia and less exercise and stress. Smoking and obesity did not seem to be important risk factors in this study, and were considered in some other studies [12]; however, a report from [13] found that smoking was associated with a higher risk of developing diabetes mellitus. The fact fewer people smoked in the group we studied might be responsible for the above finding [13].
As expected, the uncontrolled patients who did not take regular daily medications and those with as well as those patients they not on regular ophthalmological follow up were at a higher significant risk of developing DR [14]. In the current study, diabetic patients with a long duration of diabetes (10 and 15 years) were at the highest risk for developing DR. The same has been documented in other studies [15].
Concerning the distribution and grading of the retinopathy, the results we obtained from our study are consistent with many other studies, but in our finding, the frequency of proliferative retinopathy is higher in our study than the other studies [16] in the current study revealed proliferative diabetic retinopathy prevalence that was higher to the (KSA) study and also higher than that reported from the Ethiopia [16].
One of the complications of diabetes that can lead to blindness is diabetic retinopathy. The first 10 years following a diabetes diagnosis have been designated by a significant decline in visual acuity [17]. Our study’s findings support the majority of previous studies in showing that retinopathy worsens with a prolonged period of diabetes. Individuals who have just received a clinical type 2 diabetes diagnosis should be informed that even though age-related vision loss is inevitable, additional diabetes-related vision loss can be largely avoided with careful ophthalmological monitoring and surgical intervention.
Diabetes control, which includes routine doctor visits, a nutritious diet, exercise, and early management with retinal laser photocoagulation and anti-VEGF therapy, is one strategy to lessen vision loss from diabetic retinopathy.
In addition, patients with type 1 DM were at higher risk of developing DR (87.5%). The same has been documented in Saudi Arabia [18] and Ethiopia [19]. The mechanism of the association between DR and insulin use is still unclear.
Despite the improvements in health care services, DR is still a leading cause of reduced daily life activity and emotional distress due to visual acuity impairment.
DR is a serious problem, 40 years patients and older with diabetes have sight-threatening DR. Early detection and treatment of DR can save vision. For that, we need to plan DR services to avoid complications of DR as vision loss, and to health strategy to improve the management of diabetes to decrease the risk of DR.
- Ahmed RA, Khalil SN, Al-Qahtani MA. Diabetic retinopathy and the associated risk factors in diabetes type 2 patients in Abha, Saudi Arabia. J Fam Community Med. 2016;23(1):18-24. Available from: https://doi.org/10.4103/2230-8229.172225
- Aiello LP, Gardner TW, King GL, Blankenship G, Cavallerano JD, Ferris FL 3rd, et al. Diabetic retinopathy. Diabetes Care. 1998;21:143-156. Available from: https://doi.org/10.2337/diacare.21.1.143
- Alali NM, Albazei A, Alotaibi HM, Almohammadi AM, Alsirhani EK, Alanazi TS, et al. Diabetic retinopathy and eye screening: diabetic patients' standpoint, their practice, and barriers; a cross-sectional study. J Clin Med. 2022;11:6351. Available from: https://doi.org/10.3390/jcm11216351
- Alemu Mersha G, Alimaw YA, Woredekal AT. Prevalence of diabetic retinopathy among diabetic patients in Northwest Ethiopia—A cross-sectional hospital-based study. PLoS ONE. 2022;17(1). Available from: https://doi.org/10.1371/journal.pone.0262664
- Alharbi AMD, Alhazmi AMS. Prevalence, risk factors, and patient awareness of diabetic retinopathy in Saudi Arabia: a review of the literature. Cureus. 2020;12(12). Available from: https://doi.org/10.7759/cureus.11991
- Ashraf M, Sampani K, Rageh A, Silva PS, Aiello LP, Sun JK. Interaction between the distribution of diabetic retinopathy lesions and the association of optical coherence tomography angiography scans with diabetic retinopathy severity. JAMA Ophthalmol. 2020;138(12):1291-1297. Available from: https://doi.org/10.1001/jamaophthalmol.2020.4516
- Fong DS, Aiello LP, Ferris FL, Klein R. Diabetic retinopathy. Diabetes Care. 2004 Oct;27(10):2540. Available from: https://doi.org/10.2337/diacare.27.10.2540
- Flaxel CJ, Adelman RA, Bailey ST, Fawzi A, Lim JI, Vemulakonda GA, et al. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology. 2020 Jan;127(1). Available from: https://doi.org/10.1016/j.ophtha.2019.09.025
- Hafeez M, Achar P, Neeralagi M, Naik GT. Correlation between diabetic retinopathy and diabetic peripheral neuropathy in patients with type II diabetes mellitus. J Pharm Bioallied Sci. 2022;14(Suppl 1). Available from: https://doi.org/10.4103/jpbs.jpbs_138_22
- Hassan MHH, Selim KM, Hodeeb AE, din El-Ghoneimy HME, et al. Evaluation of the choroid in patients with non-proliferative diabetic retinopathy by optical coherence tomography angiography (OCTA). Al-Azhar Int Med J. 2023;4(1):11. Available from: https://aimj.researchcommons.org/cgi/viewcontent.cgi?article=1625&context=journal
- El-Bab MF, Shawky N, Al-Sisi A, Akhtar M. Retinopathy and risk factors in diabetic patients from Al-Madinah Al-Munawarah in the Kingdom of Saudi Arabia. Clin Ophthalmol. 2012;6:269-276. Available from: https://doi.org/10.2147/opth.s27363
- Li X, Xie J, Zhang L, et al. Differential distribution of manifest lesions in diabetic retinopathy by fundus fluorescein angiography and fundus photography. BMC Ophthalmol. 2020;20:471. Available from: https://bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-020-01740-2
- Moudgil T, Bains BK, Bandhu S, Kanda N. Preferred practice pattern of physicians regarding diabetic retinopathy in diabetes mellitus patients. Indian J Ophthalmol. 2021;69(11):3139-43. Available from: https://doi.org/10.4103/ijo.IJO_1339_21
- Mounirou BAM, Adam ND, Yakoura AKH, Aminou MSM, Liu YT, Tan LY. Diabetic retinopathy: An overview of treatments. Indian J Endocrinol Metab. 2022;26(2):111-118. Available from: https://doi.org/10.4103/ijem.ijem_480_21
- Sahiledengle B, Assefa T, Negash W, Tahir A, Regasa T, Tekalegn Y, et al. Prevalence and factors associated with diabetic retinopathy among adult diabetes patients in Southeast Ethiopia: A hospital-based cross-sectional study. Clin Ophthalmol. 2022;16:3527-3545. Available from: https://doi.org/10.2147/OPTH.S385806
- Salem A, Alghamdi A, Tourkmani AM, Alharbi TJ, Alrsheed AB, Almadani WH. Diabetic retinopathy among 40 years and older Saudi population with diabetes in Riyadh governorate, Saudi Arabia - A population-based survey. Saudi Med J. 2021;42(6):693-697. Available from: https://doi.org/10.1016/j.sjopt.2019.03.001
- Yasir ZH, Hassan AD, Rajiv K. Diabetic retinopathy (DR) among 40 years and older Saudi population with diabetes in Riyadh governorate, Saudi Arabia - A population-based survey. Saudi J Ophthalmol. 2019;33(4):363-368. Available from: https://doi.org/10.1016/j.sjopt.2019.03.001
- Alharbi S. Challenges and opportunities for SMEs in the Saudi Arabian market: A literature review. J Small Bus Enterp Dev. 2020;27:405-424. Available from: https://www.scirp.org/reference/referencespapers?referenceid=3715172
- Alemu MM. Impact of human activities on the ecosystem services of Nech Sar National Park. In: Human activity, biodiversity and ecosystem services in protected areas. Springer; 2022;95-119. Available from: http://dx.doi.org/10.1007/978-3-030-89571-6_4